【临床病史】:患者,男性,23岁,车祸右膝受伤,活动受限。
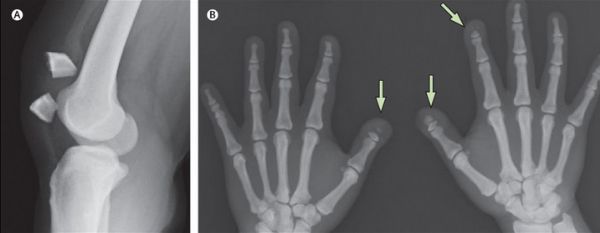
【影像图片】CR图像
 |
 |
 |
 |
【影像表现】:右侧髌骨外侧上1/ 4上下贯通。tnn影像园XCTMR.com
【影像诊断】:右侧二分髌骨 (Bipartite patella)tnn影像园XCTMR.com
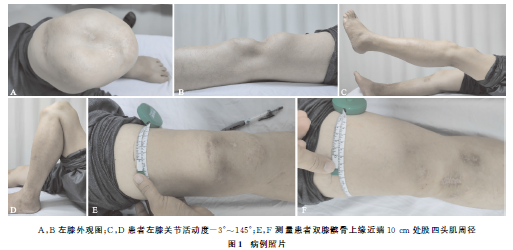
【讨论】:二分髌骨临床极少见, 在膝关节外伤或膝关节周围外伤时易诊为髌骨骨折。先天性髌骨畸形,有髌骨缺如、小髌骨、二分髌骨、三分髌等类型。髌骨是人体中最大的籽骨 ,在出生时完全为透明软骨构成,2~5 岁时出现骨化中心,17~18 岁骨化完成,髌骨一般只有一个骨化中心,但有时可以有一个或数个次级骨化中心,在 10~14 岁时出现,次级骨化中心一般在15 岁左右即愈合。tnn影像园XCTMR.com
二分髌骨乃少年阶段髌骨发育异常,出现1 个或 2 个副骨化中心,常见于髌骨外侧髌骨上1/ 4、外1 /4, 且常呈双侧对称发生。而发生在中部的,分左右或上下贯通的较为少见,个别在骨发育成熟后仍不与主骨融合 。究属先天变异还是后天病变尚有不同见解。Saupe 根据副骨化核所在部位不同而分为三型:I 型骨化核位于髌骨下极,Ⅱ型位于髌骨外侧,Ⅲ型位于外上角。其中Ⅲ型最多见,占 75 %,Ⅱ型最少,只占 5 %。Ogden认为股外侧肌的慢性抗力作用于髌骨上段外侧是二分髌骨的成因。冠状分裂髌骨也有病例报道。
误诊原因分析:二分髌骨大多为膝关节外伤时摄片检查发现,但常常被误诊为髌骨骨折,分析其误诊原因:
1、询句病史查体不详细;
2、阅片不仔细或X线片质量不高, 仅凭单一体位X线片作出诊断;
3、医生对二分髌骨缺乏了解和认识;
4、忽略了患者体征与 X 线片的统一。髌骨骨折, 根据外伤史、局部压痛、髌骨异常活动、骨擦音及X 线辅助检查, 较易鉴别。临床上应注意:
①临床仔细查体, 触摸髌骨是否有裂隙, 有无异常活动及骨擦音。
②清晰的高质量的X 线片是关键, 观察髌骨间的裂隙是否光滑、整齐、骨质是否完整, 必要时还应摄对侧X线片对比或者行CT扫描加以确诊。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







非常好
46
好
42
#X线#
37
#ART#
29
#髌骨#
0
#iPS#
36
#影像诊断#
26