ARCH PATHOL LAB MED:如何在甲醛固定石蜡包埋骨髓活检中消除自发荧光?
2019-05-09 不详 网络
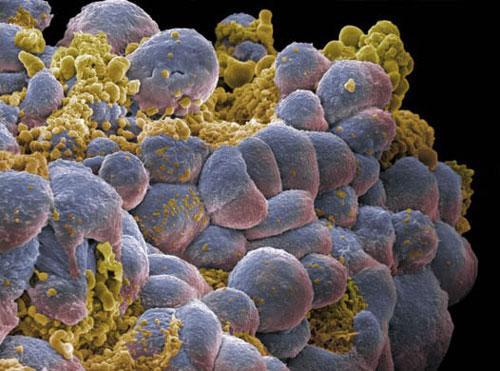
骨髓活检免疫荧光分析中骨髓组织高水平的自发荧光是检测过程的主要障碍。本研究提出一种简单、有效的骨髓活检中消除自身荧光的方法。
骨髓活检免疫荧光分析中骨髓组织高水平的自发荧光是检测过程的主要障碍。本研究提出一种简单、有效的骨髓活检中消除自身荧光的方法。
研究人员用共聚焦激光扫描显微镜观察石蜡骨髓组织在不同血液病中的自发荧光。在原发性骨髓纤维化和急性白血病中,488-nm和561-nm通道中可见强的自体荧光。为了消除自体荧光,在不同培养时间的骨髓切片上使用自体荧光猝灭剂。采用不同荧光团标记的抗体,研究了自荧光猝灭剂对骨髓活检免疫荧光分析的影响。
自荧光猝灭剂彻底消除了骨髓的强自荧光,但没有降低荧光团的强度,使靶蛋白的特异性信号清晰可见。
本研究提出了一种简单有效的骨髓石蜡组织自荧光消除方法,为骨髓活检免疫荧光分析提供了更好的方法。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Pathol#
35
#荧光#
29
#骨髓活检#
41
#甲醛#
57
#活检#
31
#Med#
26