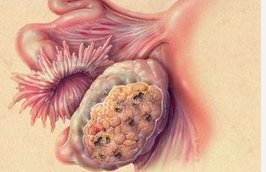
IJC:月经不规则可能增加卵巢癌风险?
2016-04-28 佚名 生物谷
最近一项研究表明,月经周期紊乱的女性晚年发生卵巢癌以及因卵巢癌死亡的风险更高。这项研究首次表明女性月经周期在非正常情况下变长或无月经与卵巢癌风险增加之间存在关联,同时对之前关于随着女性排卵总数增加,卵巢癌风险也逐渐增加的假说提出了挑战。 相关研究结果发表在国际学术期刊International Journal of Cancer上。

最近一项研究表明,月经周期紊乱的女性晚年发生卵巢癌以及因卵巢癌死亡的风险更高。这项研究首次表明女性月经周期在非正常情况下变长或无月经与卵巢癌风险增加之间存在关联,同时对之前关于随着女性排卵总数增加,卵巢癌风险也逐渐增加的假说提出了挑战。
相关研究结果发表在国际学术期刊International Journal of Cancer上。
普遍认为排卵周期少是避免卵巢癌的一种保护性因素。因此服用特定类型的避孕药,妊娠以及输卵管结扎等终止排卵的措施也被认为能够帮助降低卵巢癌风险。
虽然在所有患癌女性中,卵巢癌患者仅占3%,但卵巢癌是所有妇科癌症中的头号杀手。所有诊断为卵巢癌的女性中只有不到一半的病人存活超过5年。一些卵巢癌的早期症状经常被病人忽视或被误诊为其他疾病,并且目前还没有用于卵巢癌常规筛查的方法和标记物,因此多数病人发现病情的时候已经错过最佳治疗时机。
为了找到除年龄和遗传之外的风险因素,流行病学家Barbara Cohn以及她带领的研究团队对1959年一项关于女性妊娠的大型研究的数据进行了深入分析,该研究包含了来自美国加州的超过15000名女性。研究人员期望能够对母女在一生中罹患卵巢癌的风险进行追踪。在这项大型研究刚开始的时候即有大约13%的女性存在月经周期紊乱的情况(一个月经周期的时间超过35天或者长期出现月经周期少或无经),当时参与研究的女性平均年龄为26岁。
在接下来的50年中,有116名女性患卵巢癌,其中84人死于卵巢癌。到参与者70岁的时候,有月经周期紊乱情况的女性罹患卵巢癌以及死于卵巢癌的风险接近正常女性的两倍,这种关联性只随年龄增长而变强。举例来说,到女性年龄达到77岁的时候,有月经周期紊乱情况的女性罹患卵巢癌以及死于卵巢癌的风险大约是正常女性的三倍。
这些卵巢癌患者中许多人同时存在多囊卵巢综合征(PCOS),而PCOS患者经常存在月经周期紊乱或无经的情况,研究人员认为PCOS可能是促进卵巢癌发生的一个重要原因,但由于PCOS的诊断标准出现在该研究开始以后,因此无法根据这项研究的结果得出两者之间的确切关系。
研究人员表示,这项研究的结果对未来研究有一些指导意义,不仅能够帮助发现卵巢癌高风险人群还可以告诉人们哪些女性能够通过筛查或预防措施受益。
原始出处:
Cirillo PM, Wang ET, Cedars MI, Chen LM, Cohn BA. Irregular menses predicts ovarian cancer: Prospective evidence from the Child Health and Development Studies. Int J Cancer. 2016 Apr 15. doi: 10.1002/ijc.30144
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










深度好文,值得关注
57
#癌风险#
28
学习啦!
137
#月经#
23
学习了,卵巢癌现在也多发
133