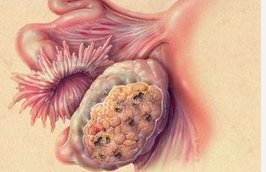
JCO:卵巢癌新药Farletuzumab三期临床试验结果发表,3年前已完成试验,结果阴性
2016-03-29 MedSci MedSci原创
Farletuzumab是一种人源化的单克隆抗体,其靶点为叶酸受体α。叶酸受体α在卵巢癌中高度表达而在大部分正常组织中并不存在。Farletuzumab目前处于双盲、随机的三期临床试验中,用于治疗对铂敏感性卵巢癌。 符合试验条件的患者是在经过铂-紫杉烷化疗完成后出现首次复发6-24个月。所以的患者均接受卡铂加紫杉醇或者多系紫杉醇(六个循环结合随机分配的测试药物,比例为1:1:
Farletuzumab是一种人源化的单克隆抗体,其靶点为叶酸受体α。叶酸受体α在卵巢癌中高度表达而在大部分正常组织中并不存在。Farletuzumab目前处于双盲、随机的三期临床试验中,用于治疗对铂敏感性卵巢癌。

实际上,2013年,卫材公司(Eisai)研究就完成,但到现在才正式公开发表出来。Farletuzumab(MORAb-003),在用于对铂类敏感的上皮性卵巢癌患者的首次复发治疗的Ⅲ期临床 FAR 131 研究未达到无进展生存期(PFS)的主要观察终点。全球每年约有 14 万人死于卵巢癌,90%的癌变肿瘤往往是因为没有及时确诊。虽然很多患者接受了手术和化疗,但复发仍十分普遍。
原始出处:
Vergote I, Armstrong D, Scambia G, et al. A Randomized, Double-Blind, Placebo-Controlled, Phase III Study to Assess Efficacy and Safety of Weekly Farletuzumab in Combination With Carboplatin and Taxane in Patients With Ovarian Cancer in First Platinum-Sensitive Relapse[J]. Journal of Clinical Oncology, 2016: JCO632596.本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mAb#
28
#三期临床试验#
26
#三期临床#
30
#JCO#
34
#卵巢癌新药#
32