PLoS One:急性缺血性脑卒中患者,高血浆hsCRP水平与不良临床预后独立相关
2016-06-30 phylis 译 MedSci原创
背景:尽管由于脑梗死后炎症反应使得血浆C反应蛋白(CRP)升高,但急性缺血性卒中后的C反应蛋白与临床预后的关系仍不明朗。本研究旨在探讨血浆高敏C反应蛋白(hsCRP)水平是否独立于传统的危险因素和急性卒中后感染,与临床结局相关。方法:研究者前瞻性纳入3653例首发缺血性脑卒,这些患者功能独立,并且症状开始24h内入院。入院时检测血浆hsCRP水平,将血浆hsCRP水平分为四分位数。采用Logist
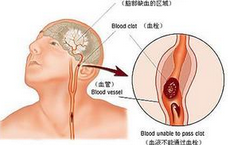
背景:尽管由于脑梗死后炎症反应使得血浆C反应蛋白(CRP)升高,但急性缺血性卒中后的C反应蛋白与临床预后的关系仍不明朗。本研究旨在探讨血浆高敏C反应蛋白(hsCRP)水平是否独立于传统的危险因素和急性卒中后感染,与临床结局相关。
方法:研究者前瞻性纳入3653例首发缺血性脑卒,这些患者功能独立,并且症状开始24h内入院。入院时检测血浆hsCRP水平,将血浆hsCRP水平分为四分位数。采用Logistic回归分析hsCRP水平与临床预后的相关性,包括神经功能改善,神经功能恶化和不良的功能预后(3个月内改良Rankin量表≥3)。
结果:校正了年龄、性别、基线国立卫生研究院卒中量表评分、卒中的亚型,传统的危险因素,静脉溶栓和介入治疗,住院期间急性感染后,较高的hsCRP水平与不良结果明显相关(最高四分位数与最低四分数数相比,神经功能改善多变量aOR [ 95%CI ]:0.80 [ 0.65-0.97 ],神经恶化aOR 1.72 [1.26-2.34 ],功能预后不良2.03 [1.55-2.67 ])。校正住院期间感染,卒中再发或死亡的患者后,这种相关性仍存在。不管卒中亚型或基线卒中严重程度,这种趋势是相似的,在年龄小于70岁中更显著。
结论:急性缺血性脑卒中患者,高血浆hsCRP水平与不良临床预后独立相关。
原始出处:
Matsuo R, Ago T, et al. Plasma C-Reactive Protein and Clinical Outcomes after Acute Ischemic Stroke: A Prospective Observational Study. PLoS One.Jun,2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#卒中患者#
33
#缺血性脑#
36
#缺血性#
35
#脑卒中患者#
39
#HSC#
0
拜读了,受益匪浅,点个赞!
71
#CRP水平#
29
#Plos one#
26
#急性缺血性脑卒中#
26
#CRP#
29