Am J Transplant:供者BMI>30—活体肝捐献的禁忌证?
2017-04-18 吴刚 环球医学
肝移植是各种终末期肝病最有效的治疗方法。2017年3月,发表在《Am J Transplant》的一项由加拿大和德国科学家进行的研究表明,供者BMI>30并非活体肝捐献的禁忌证。 世界上,肥胖症患病率的增加威胁了活体肝供者的来源。虽然移植物脂肪变性对肝脏捐献和移植的负面影响众所周知,但是在没有肝脏脂肪变性的情况下,肥胖对活体供者肝移植(LDLT)结局的影响未知。因此,研究人员比较了BMI<30和
肝移植是各种终末期肝病最有效的治疗方法。2017年3月,发表在《Am J Transplant》的一项由加拿大和德国科学家进行的研究表明,供者BMI>30并非活体肝捐献的禁忌证。
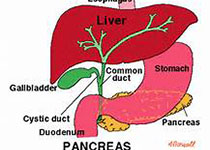
世界上,肥胖症患病率的增加威胁了活体肝供者的来源。虽然移植物脂肪变性对肝脏捐献和移植的负面影响众所周知,但是在没有肝脏脂肪变性的情况下,肥胖对活体供者肝移植(LDLT)结局的影响未知。因此,研究人员比较了BMI<30和BMI≥30的供者的LDLT结局。
2000年4月~2004年5月,105名患者从BMI≥30的供者中接受了肝右叶移植,364名受者从BMI<30的供者中接受了移植物。通过影像学和肝脏活检,所有BMI>30的供者,排除了肝脏脂肪变性>10%。供者不具有任何其他的合并症。BMI<30和BMI≥30的供者具有相似的术后并发症发生率(Dindo-Clavien≥3b:2% vs 3%;P=0.71)和住院日(6 vs 6天;P=0.13)。通过移植后血清胆红素峰值和国际标准化比率评估的受者移植物功能完全相同。此外,组间受者并发症发生率(Dindo-Clavien≥3b:25% vs 20%;P=0.3)或住院日没有差异。
研究人员得出结论,BMI≥30的供者在没有移植物脂肪变性的情况下,对LDLT不禁忌。
原始出处:
Knaak M, Goldaracena N, Doyle A, Cattral MS,et al. Donor BMI >30 Is Not a Contraindication for Live Liver Donation. Am J Transplant. 2017 Mar.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#捐献#
27
#Transplant#
25
#plant#
33
#TRA#
23
#禁忌#
27
学习了,谢谢分享
40