Lancet:震惊!PD-1/PD-L1免疫抑制剂或可出现致死性并发症!
2018-03-19 Michael,Yui 转化医学网
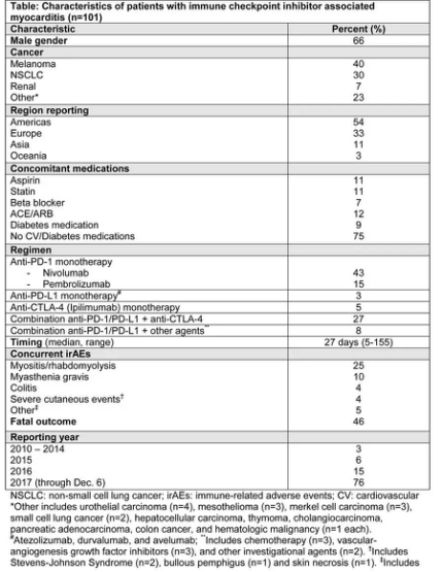
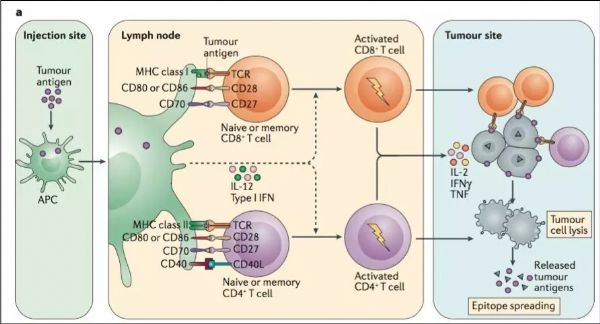
免疫检查点抑制剂极大地改善了多种癌症类型的临床结果,并越来越多地用于早期疾病和其他疗法。但是,这可能导致高度免疫相关的不良事件。暴发性免疫检查点抑制剂相关性心肌炎已经有相关机构报道,但这个新临床病例的临床特征,出现时机和预后是尚不明确。研究人员使用VigiBase(世卫组织个人病例安全报告数据库)明确了101例使用免疫检查点抑制剂后出现严重心肌炎的病例。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
18
#并发#
20
#抑制剂#
34
#PD-L1#
22
#免疫抑制剂#
35
#致死性#
28
学习了.谢谢分享
57
不错耶.学习了
64
学习了.谢谢分享.
70
^_^^_^^_^
54