Neurology:大面积急性缺血性卒中患者血管内取栓术与功能预后的关系
2022-09-01 Naomi MedSci原创
近日,一项发表在Neurology上的研究发现,在基线CTP缺血核心容量为70-100毫升的患者中,EVT与卒中后3个月的预后呈正相关,而在≥100毫升的患者中则不然。需要随机数据来证实这些发现。
血管内血栓切除术(EVT)对CT灌注(CTP)确定的缺血核心体积较小的大血管闭塞(LVO)卒中患者是有效的。然而,对于核心容量>70ml的患者,EVT的益处尚不清楚。近日,一项发表在Neurology上的研究比较了核心≥70ml的EVT和非EVT患者的预后,假设卒中后三个月的改良朗肯分级(MRS,0-3)对EVT患者的预后有好处。
研究人员回顾分析在多中心(澳大利亚、中国和加拿大)登记的患者(2012年至2020年),这些患者在卒中发病24小时内接受了CTP,且基线缺血核心≥70ml。主要结果是对核心容量≥70ml的患者以及70-100ml和≥100ml亚组患者的EVT与预后良好的相关性进行评估。
- 在登记的3283例患者中,299例核心≥70ml,269例数据完整(135例核心容量在70-100ml~134≥100ml之间)。
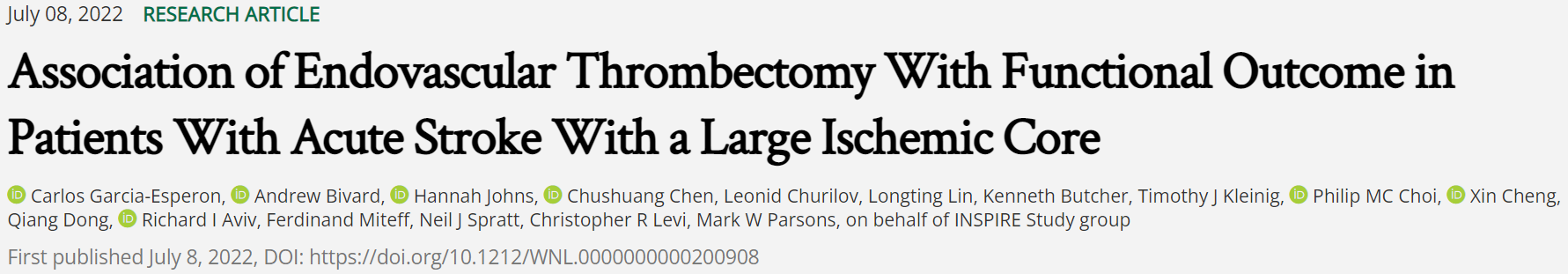
- 121例(45%)患者行EVT。接受EVT治疗的患者更年轻(中位数69岁对75岁;p=0.011),卒中前MRS较低,核心体积中位数较小,92[79-116.5]毫升对105.5[85.75138]毫升(p=0.004)。
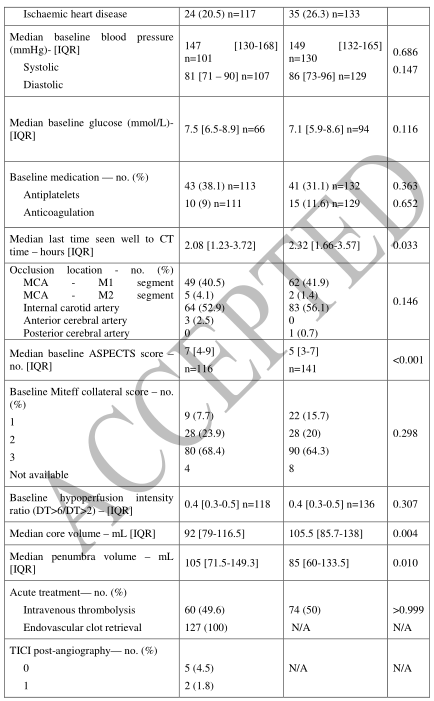
- 在调整后的分析中,接受EVT治疗的患者获得良好结果的几率更高(非EVT组为30%比13.9%;AOR2.1(95%CI 1,4.2),p=0.038)。
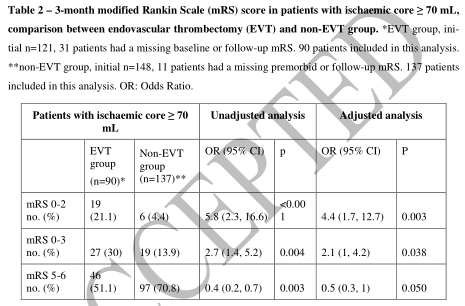
- 受益主要见于70-100ml核心的患者(71/135(52.6%)接受EVT治疗),其中接受EVT治疗的54.3%与非EVT组的21%取得了良好的结果(AOR2.5(95%可信区间1,6.2),p=0.005)。
- 在核心缺血体积≥100ml的患者中,50例(37.3%)接受了EVT。
- 两组患者的公平结局比例都非常低(8.1%对8.7%;p=0.908)。
研究发现,在基线CTP缺血核心容量为70-100毫升的患者中,EVT与卒中后3个月的预后呈正相关,而在≥100毫升的患者中则不然。需要随机数据来证实这些发现。
证据分类这项研究提供了III类证据,证明在核心为70-100毫升的CTP定义的缺血性卒中后3个月,EVT与更好的运动结果有关。
文献来源:Garcia-Esperon C, Bivard A, Johns H, et al. Association of Endovascular Thrombectomy With Functional Outcome in Patients With Acute Stroke With a Large Ischemic Core [published online ahead of print, 2022 Jul 8]. Neurology. 2022;10.1212/WNL.0000000000200908. doi:10.1212/WNL.0000000000200908
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#缺血性卒#
43
#缺血性#
45
#大面积#
53
#Neurol#
39
#卒中患者#
32
#缺血性卒中患者#
45
#取栓术#
0
#取栓#
48
#功能预后#
39
谢谢
39