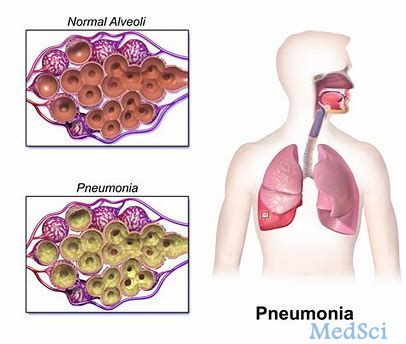
AR-105治疗呼吸机相关性肺炎(VAP)的中期研究未能达到主要终点
2019-09-04 Allan MedSci原创
Aridis制药公司报道,用于治疗由革兰氏阴性铜绿假单胞菌引起的呼吸机相关性肺炎(VAP)的实验药物AR-105的II期研究未能达到主要终点。
Aridis制药公司报道,用于治疗由革兰氏阴性铜绿假单胞菌引起的呼吸机相关性肺炎(VAP)的实验药物AR-105的II期研究未能达到主要终点。该试验随机分配了158例VAP患者,接受安慰剂或AR-105治疗。该研究的主要终点是AR-105治疗后第21天的临床肺炎治愈率,而次要终点包括第7、14、28天的临床肺炎治愈率,全因死亡率和若干健康经济学参数。
Aridis制药公司指出,研究调查人员或试验数据监测委员会未发现与AR-105有关的严重不良事件或死亡事故。然而,根据结果,制药商表示将不再投入资源来开发AR-105。首席医疗官Wolfgang Dummer说:“我们的团队正在分析完整的数据集,并尽快报告最终分析结果”。
原始出处:
http://www.firstwordpharma.com/node/1663369#axzz5yVqufGke
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#AR-105#
32
#主要终点#
34
#相关性#
33
#VAP#
0
#呼吸机#
25