3D打印“骨骼”的应用
2015-02-09 孙凯 杜卉 整理 中国医学论坛报
2014年8月,美国食品与药物管理局(FDA)首次批准OsteoFab患者特异性面部装置(OPSFD,图2a)为用于面部重建的3D打印聚合置入物。OPSFD是以磁共振成像(MRI)或CT扫描结果为模板,针对患者的个体化解剖情况而生产的面部置入物。该3D打印聚合置入物具有生物相容性,呈透明状态,并以能支撑骨附着等多种方式与骨类似。 同月,我国一名12岁因外伤致恶性肿瘤的男孩儿

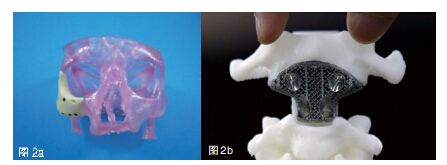
2014年8月,美国食品与药物管理局(FDA)首次批准OsteoFab患者特异性面部装置(OPSFD,图2a)为用于面部重建的3D打印聚合置入物。OPSFD是以磁共振成像(MRI)或CT扫描结果为模板,针对患者的个体化解剖情况而生产的面部置入物。该3D打印聚合置入物具有生物相容性,呈透明状态,并以能支撑骨附着等多种方式与骨类似。
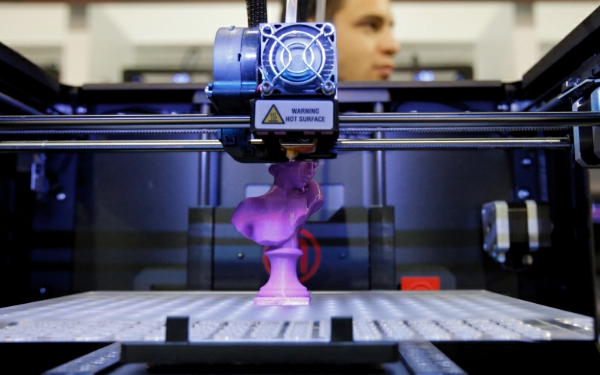
同月,我国一名12岁因外伤致恶性肿瘤的男孩儿,在北京大学第三医院接受了全球首个3D打印的脊柱(图2b)置入术,以预防肿瘤的播散。3D打印机可以生成非常复杂的几何形状,这意味着为固定置入物所需要的附加硬件数量可以减少。另一个益处是,打印置入物的多孔性可以使骨在置入物内生长进而形成一种自然的连结。除了脊柱置入物,北京大学第三医院还用3D打印技术制作椎间盘。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









高端大气
100
患OS这个疾病的高风险人群提供干预措施以避免不良预后和机械治疗措施
110
长知识了!谢谢!
143
?学习了
115
已阅
110
外伤导致的恶性肿瘤?
127
#3D#
24