Circulation:早期心律控制有助于减少多合并症的新发房颤患者的心血管结局
2022-09-16 MedSci原创 MedSci原创
近期确诊的 CHA2DS2-VASc 评分≥4分的心房颤动患者应考虑进行早期心律控制以减少心血管不良结局
随机的 EAST-AFNET4 试验显示,早期心律控制 (ERC) 可减少近期确诊的有卒中危险因素的心房颤动患者的不良心血管结局。但是,迄今为止,ERC 在患有多种心血管合并症的患者中的有效性和安全性尚不清楚。
本次 EAST-AFNET4 试验预定的亚组分析比较了 ERC 与常规治疗(UC)在 CHA2DS2-VASc 评分≥4分和低合并症负担的患者中的效果和安全性。
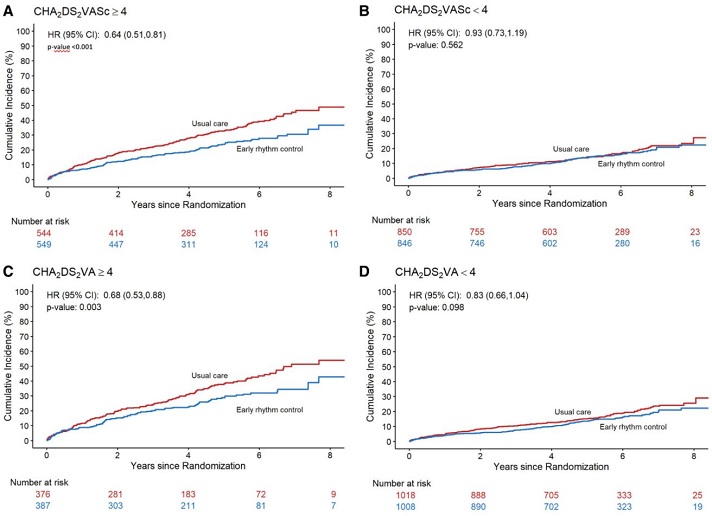
在 EAST-AFNET4 试验中,1093位 CHA2DS2-VASc 评分≥4分的患者(74.8±6.8岁,61%的女性)和1696位 CHA2DS2-VASc 评分<4分的患者(67.4±8.0岁,37%的女性)被随机分至两组。与 UC 相比,ERC 减少了CHA2DS2-VASc 评分≥4分的患者的心血管死亡、卒中或心衰加重或急性冠脉综合征住院的复合主要疗效结局(ERC组,127/549例事件;UC组,183/544例事件;HR 0.64, P<0.001),但两组 CHA2DS2-VASc 评分<4分的患者之间无此差异(122/846 vs 133/850;HR 0.93,P=0.56)。
两组主要结局的累积发生率
两组 CHA2DS2-VASc 评分≥4分的患者之间的主要安全终点(死亡、卒中或心律控制治疗的严重不良事件)无显著差异(112/549 vs 132/544;HR 0.84, P=0.175),但接受 ERC 治疗的 CHA2DS2-VASc 评分<4分的患者的不良事件较 UC 组更常见(119/846 vs 91/850;HR 1.39,P=0.019)。两组间危及生命的事件或死亡事件没有差异。
综上,近期确诊的 CHA2DS2-VASc 评分≥4分的心房颤动患者应考虑进行早期心律控制以减少心血管不良结局,而合并症较少的患者可能不能从早期心律控制中显著获益。
原始出处:
Andreas Rillig, et al. Early Rhythm Control in Patients With Atrial Fibrillation and High Comorbidity Burden. Circulation. 2022;146:836–847. https://doi.org/10.1161/CIRCULATIONAHA.122.060274
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#合并症#
40
#心血管结局#
73
#新发房颤#
46
#房颤患者#
44