专家访谈:王伟民:光学相干断层成像OCT助力实现钙化病变介入治疗效果更优化
2021-01-04 《门诊》杂志 门诊新视野
钙化病变是广大临床医生在冠脉介入治疗中需要攻克的一大难点。其相较于其他病变,器械通过更为困难,常常无法充分预处理,会造成术中和术后各类并发症,影响患者的预后。
钙化病变是广大临床医生在冠脉介入治疗中需要攻克的一大难点。其相较于其他病变,器械通过更为困难,常常无法充分预处理,会造成术中和术后各类并发症,影响患者的预后。随着影像学技术的推广应用,使得对钙化病变的充分判断和处理成为可能。近日,《门诊》杂志特邀北京大学人民医院王伟民教授结合冠脉钙化病变的特点及OCT领域最新进展,畅谈OCT在钙化病变治疗策略制定方面的作用及未来发展前景。
钙化病变是介入治疗的一大难点
钙化病变的发病率约30%,目前仍是广大术者临床实践中需要攻克的难题。尤其对于复杂高危(CHIP)患者,严重的钙化病变增加了手术难度,请您谈谈钙化病变对介入治疗带来了怎样的影响?针对其治疗需要注意些什么?
王伟民教授:临床中,钙化病变约占冠脉病变的三分之一,其中严重钙化病变约为6%。流行病学资料显示,患者冠状动脉狭窄程度越高,伴有钙化的概率越大;此外,高龄、脂质代谢异常、糖尿病、慢性肾病、肾透析等患者是冠状动脉钙化病变的高发人群,病变钙化程度往往较为严重。随着中国人口老龄化进程加快,合并有糖尿病、高血压、慢性肾病等患者数量的不断增加,冠脉严重钙化病变比例也越来越高,而冠脉钙化病变的存在,可显著增加PCI的难度和风险,尤其是存在严重钙化病变的患者,手术即刻的并发症以及早期和晚期主要不良心血管事件的发生率明显升高。
在心血管内科,有句俗语:“天不怕地不怕,就怕冠脉有钙化”;冠脉钙化病变经常贯穿于各种复杂病变,大大增加了冠脉介入治疗的难度。首先,钙化病变的存在可增加介入相关器械通过的难度,增加PCI相关并发症,如介入器械不能到位、支架脱落、导丝断裂等风险的发生。其次,钙化病变属于高阻力病变,球囊有时难以充分扩张,甚至会发生球囊破裂等情况;当需要较高的压力扩张钙化病变时,患者发生血管夹层、穿孔、破裂、无复流等事件的概率明显增加。最后,在未充分扩张的钙化病变段内植入支架,容易出现支架膨胀不全、贴壁不良、支架不规则变形等,从而增加后期支架内血栓、支架再狭窄等风险。因此,正确的识别、评估钙化病变,选择恰当的介入治疗技术,对于提高手术成功率、减少手术相关并发症、改善患者近、远期预后具有非常重要的作用。
腔内影像技术“助力”钙化病变诊疗
腔内影像学技术的出现为临床治疗提供了重要指导。OCT或IVUS在指导钙化病变中各有何特点?可为术者提供哪些有用信息,从而帮助术者优化治疗?
王伟民教授:近20年来,腔内影像学技术取得了长足的进步和发展,在复杂冠脉病变中,腔内影像学技术可作为良好的补充,指导冠脉介入治疗。血管内超声成像(IVUS)和光学相干断层成像(OCT),作为当前主流的两种腔内影像学技术,有着不同的技术特点和优势,在钙化病变介入诊疗中均扮演着十分重要的角色。
IVUS对于检出钙化病变具有较高的敏感性,可较好地判断钙化在血管里的分布位置和范围,以帮助介入治疗策略的制定。与IVUS相比,OCT具有更高的成像分辨率,既可以精确地检出钙化病变,亦可对钙化病变的分布区域、面积和体积进行精确测量,提供更为准确、全面的钙化信息,从而更精准地指导PCI治疗。例如,当术前OCT检查发现严重的环状钙化时,应避免直接置入支架,可进行充分旋磨后,再行球囊扩张并植入支架;术中可应用OCT观察旋磨后钙化环前后的变化,如钙化环出现薄弱环节或分离,则表明旋磨取得满意效果,可使用非顺应性球囊扩张;如未出现薄弱环节或者旋磨效果不满意,则可选择进一步进行旋磨处理。
总而言之,OCT不但可以充分评估钙化病变的性质和严重程度,而且在钙化病变PCI中,可以在各个环节帮助临床医师进行决策,在OCT支持下,临床医师可进行更为充分的术前评估,并指导术中操作,积极改善患者预后,辅助临床医师最终取得满意的临床疗效。
OCT优化钙化病变介入诊疗标准路径
通过临床实践的不断地积累,总结出一套“OCT优化钙化病变介入诊疗标准路径”,能否请您介绍一下此路径的特点?同时,您如何看待LIGHTLAB研究结果对国内临床实践的指导意义?
王伟民教授:近期发布的LIGHTLAB研究结果表明,标准化OCT指导可以改变88%的临床治疗策略;在血管预处理方面,OCT改变了28%的血管预处理策略,其中约3/4的策略变化发生在钙化病变,成功展示了OCT技术对钙化病变介入策略制定的指导价值。此外,值得注意的是,该研究全程采用了一套标准治疗流程指导和优化PCI,即OCT优化PCI标准治疗路径——MLD MAX,重点强调了术前策略制定、术后评估及优化的流程及要点;MLD MAX可给国内临床实践的开展带来一定启示,广大临床医师应在此基础上,积极总结国内外经验,并根据国内患者的具体情况作出最为恰当的处理措施。
冠脉旋磨是当前临床医师处理严重钙化病变的主要手段之一,本中心作为国内最早开展该技术的综合医院之一,病例总量位居国内前列,病变复杂程度更是名列前茅,在此基础上,本中心在不断深入认识钙化病变形成机制,以及应用OCT指导钙化病变治疗的过程中,通过观察、总结、探讨,逐渐摸索出一套“OCT优化钙化病变介入诊疗标准路径”。本路径基于中国患者数据,对于国内钙化病变的介入治疗提供了一定的参考。相较于国外路径,本路径首次制定了处理钙化结节的标准路径,并建议临床医师只要发现患者存在严重钙化病变,或存在钙化结节,就应采取旋磨治疗,不应忽略钙化结节对患者预后及支架植入存在的影响。此外,基于本中心的临床经验,“OCT优化钙化病变介入诊疗标准路径”建议当钙化病变厚度在0.6 mm-0.8 mm时,可通过应用切割球囊、棘突球囊甚至非顺应性高压球囊等,打开钙化环,进行后续操作;相较于国外临床研究中单纯以0.6 mm为界值,判断是否需要继续旋磨,更为精准,也更为适合广大中国患者。
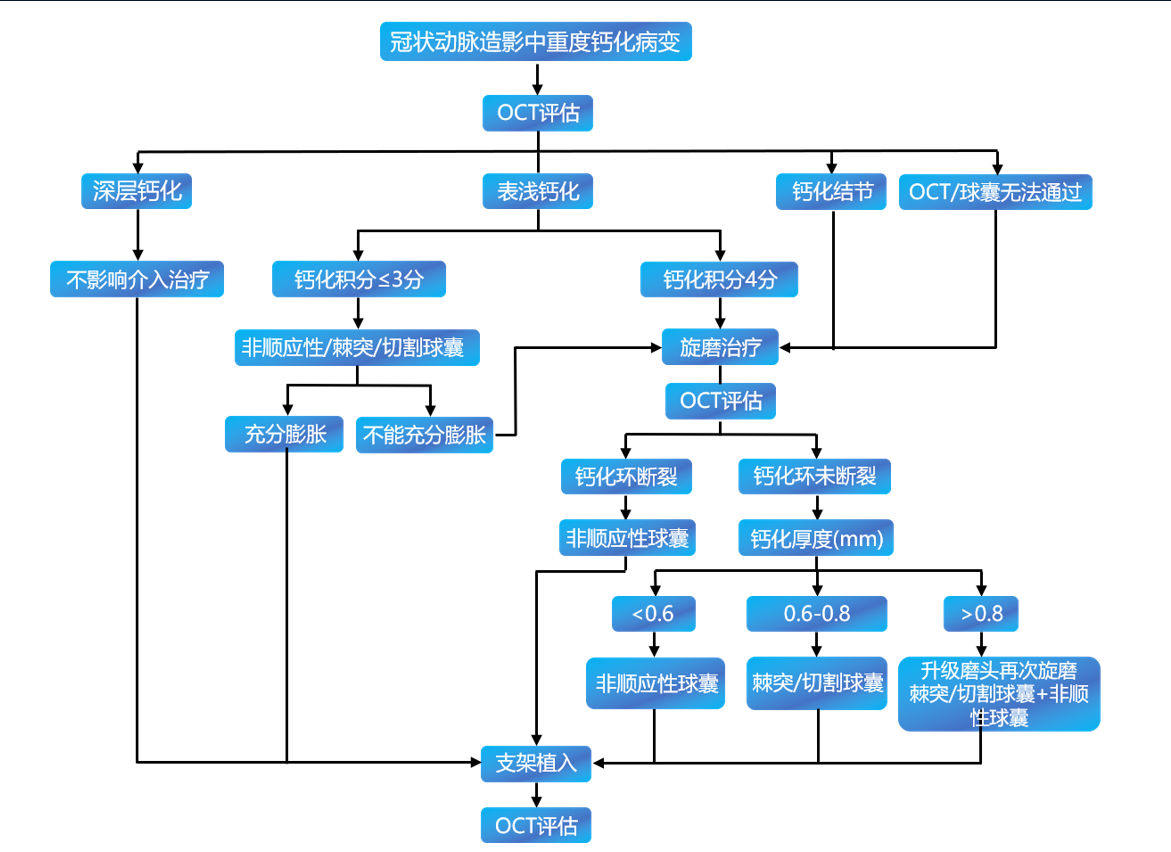
OCT优化钙化病变介入诊疗标准路径
迈向更大的舞台
目前我国OCT临床应用尚不普及,OCT渗透率仅为1%,您认为未来该如何推广OCT在我国的临床应用,让更多患者获益?您对于OCT在未来的发展有何期待?
王伟民教授:OCT有着极高的分辨率,在评价易损斑块和指导支架置入,尤其是在ACS、严重钙化病变等诊疗领域日益受到关注。目前,OCT在临床中的应用比例仍较低,且不同中心间存在较大差异,如何进一步推广OCT技术应成为下一步紧抓的要点。首先,可通过开展更多各种形式的规范教育与培训、OCT相关学术活动,增加临床医师了解、认识该项技术的机会。其次,优化操作(如充分利用造影融合功能)以减少OCT检查中的造影剂用量,为钙化程度相对较为严重的老年患者或肾功能不良患者带来更多获益。最后,正确把握影像技术适应证,根据患者个体情况及现有技术条件,合理选择影像学手段以诊断、评估冠脉钙化病变。
如今,介入治疗已迎来精准介入新时代,如何实现“优化治疗效果、减少并发症”成为所有临床医师的共同追求。然而,“精准介入”目标的实现,并非按照传统经验仅依靠肉眼,其与腔内影像学工具的支持密不可分。OCT是近年来快速发展的一种腔内影像学评估工具,凭借独特优势,可满足临床实际工作的需求,对复杂冠脉病变介入治疗具有极大的指导意义。相信随着OCT技术的不断改进和完善,操作将更加简单,并常规应用于临床,广泛应用于心血管各个领域。未来OCT技术必将被更多医师与患者认可,逐渐走向更大的舞台!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#专家访谈#
44
#钙化病#
59
#钙化病变#
50
#OCT#
43
#治疗效果#
48
很棒,获益良多,终身学习。
73
学习了,涨知识了!
79
认真学习了
75
很好
74
先进技术好啊
77