Nat Commun:王凯亮/卞兆祥团队发现一种新的胰岛素抵抗调节机制和衰老相关糖尿病的治疗靶点
2022-07-04 郭轩铭 “小柯生命”公众号
2型糖尿病(T2D)是一种慢性代谢性疾病,全球约有3. 7亿成年患者。健康人群中,胰腺分泌的激素胰岛素可以调控餐后血糖。
2022年6月29日,香港浸会大学王凯亮助理教授和卞兆祥教授领导的研究小组,在《自然—通讯》(Nature Communications)发表论文。
研究团队发现了一种名为MT1-MMP的蛋白水解酶,该酶调节人类和非人类灵长类动物衰老所导致的胰岛素抵抗发展,并发现MT1-MMP可作糖尿病治疗的新靶点。
2型糖尿病(T2D)是一种慢性代谢性疾病,全球约有3. 7亿成年患者。健康人群中,胰腺分泌的激素胰岛素可以调控餐后血糖。在T2D患者中,对胰岛素敏感的组织,如肝脏和肌肉,对胰岛素则没有反应,这种现象被称为胰岛素抵抗。因此导致糖在血液中停留的时间更长,随后引发一系列与T2D相关的健康问题,包括四肢坏死、失明甚至死亡。众所周知,胰岛素抵抗和T2D的发病率随年龄增长而增加。然而,与年龄相关的胰岛素抵抗机制还不是很清楚。因此,发现特异性调控胰岛素作用因子,并研究它如何在老龄化过程中调节胰岛素敏感性,可为针对T2D和其他年龄相关代谢功能疾病的治疗提供新的见解。
胰岛素是一种激素,其通过与胰岛素受体(IR)结合向细胞发出信号,将糖从血液中排出。因此,调控IR的表达可以影响胰岛素调节血糖的能力,从而帮助维持葡萄糖平衡。以此为出发点,研究小组进行了一系列实验探究MT1-MMP对IR的调节作用。他们发现,衰老与小鼠MT1-MMP的增加和激活有关。与对照组相比,缺少MT1-MMP的老年小鼠表现出更好的胰岛素敏感性和葡萄糖耐受。此结果表明,MT1-MMP活性的增加可能是衰老所导致的胰岛素抵抗的一个风险因素,而MT1-MMP的缺失可防止小鼠免受衰老相关的胰岛素抵抗。更重要的是,在老年猴和人类样本中,研究人员也发现MT1-MMP的水平增加,这表明MT1-MMP依赖的胰岛素调节机制在脊椎动物中是保守的。
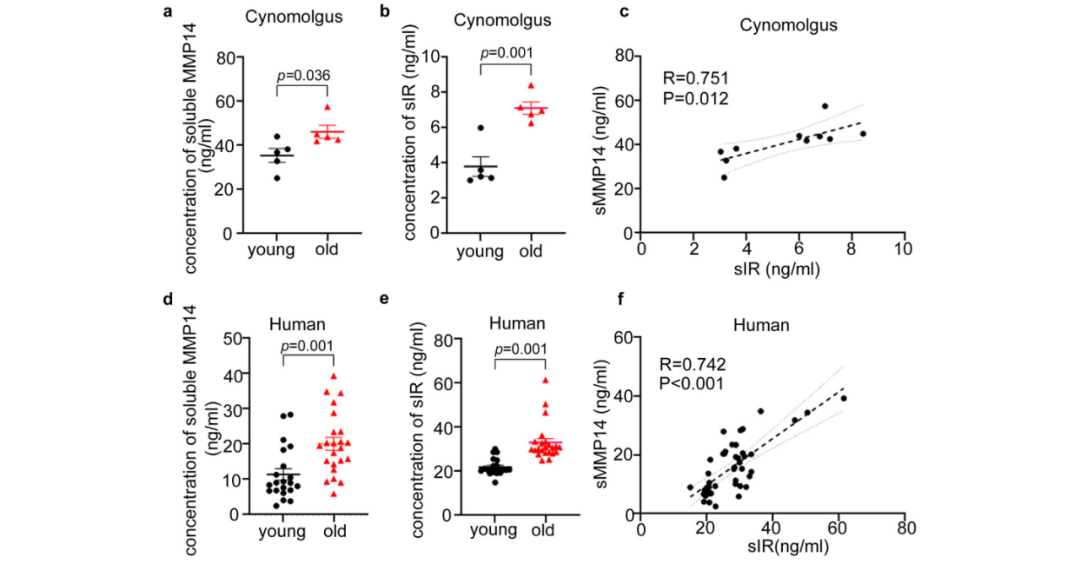
老年灵长类动物中可溶性胰岛素受体水平升高。(图源:GuoXM, et al., Nat Commun, 2022)
为了解MT1-MMP抑制胰岛素作用的具体机制,研究小组进行了一系列分子生物学,细胞生物学与动物实验。结果显示,在高表达MT1-MMP的细胞中,观察到IR的表达明显减弱,并观察到胰岛素信号的降低。其具体机制为MT1-MMP将IR从胰岛素敏感细胞的细胞膜表面剪切下来,随后阻断了胰岛素与IR的结合,从而抑制了胰岛素的信号传导。
为探索以MT1-MMP为靶点治疗糖尿病的潜力,他们发现通过一种特异性中和抗体对MT1-MMP活性进行抑制,可使各种糖尿病小鼠模型的代谢参数包括葡萄糖耐量和胰岛素敏感性得到明显改善。这些结果表明,MT1-MMP是治疗糖尿病的一个潜在药物靶点。

(图源:王凯亮实验室)
他们先前发表在《自然—代谢》(Nature Metabolism)上的研究表明,抑制MT1-MMP的活性,能够有效减少肥胖小鼠的体重增加,而肥胖是糖尿病的一个主要风险因素。因此,靶向MT1-MMP可作为治疗T2D和肥胖症的联合治疗策略。
除香港浸会大学的研究人员外,该研究团队还包括来自香港大学和美国德克萨斯大学休斯顿健康科学中心的科学家。
原始出处:
Guo, X., Asthana, P., Gurung, S. et al. Regulation of age-associated insulin resistance by MT1-MMP-mediated cleavage of insulin receptor. Nat Commun 13, 3749 (2022). https://doi.org/10.1038/s41467-022-31563-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#治疗靶点#
63
#COMMUN#
55
#胰岛#
66
#调节机制#
0
#Nat#
42