JACC:成人先天性心脏病患者左心室收缩功能障碍的患病率和预后影响
2022-04-08 网络 网络
12%的成人CHD患者存在LVSD,在右侧病变的患者中更为常见,并与心血管事件相关。
无症状性左心室收缩功能障碍(ALVSD)定义为左室收缩功能降低但无心力衰竭(HF)。通常指的是左室收缩功能降低,表现为左室射血分数(LVEF)低于正常和/或节段性室壁运动异常。
人群研究表明,ALVSD至少与射血分数降低型HF(HFrEF)一样常见。ALVSD是进展至HF和死亡的危险因素。美国心脏病学会基金会/美国心脏协会的指南中,无HF症状或体征的结构性心脏病(包括左室收缩功能障碍)被归为“B阶段HF”。
尽管左心室收缩功能障碍(LVSD)的发病率和预后影响,以及心脏治疗对LVSD的影响在后天性心脏病患者中得到了很好的描述。LVSD被定义为左心室射血分数(LVEF)<52%/<54%(男性/女性)。心血管事件被定义为心衰住院、心脏移植和心血管死亡。但在先天性心脏病(CHD)的成人中却少有研究。

为了确定LVSD的流行率、风险因素和预后影响,以及心脏疗法(指南指导下的医学治疗[GDMT]和心脏再同步化治疗[CRT])对成人CHD患者LVSD的影响。来自mayo诊所的专家对患有CHD的成年人的系统性LV的回顾性研究,结果发表在JACC杂志上。
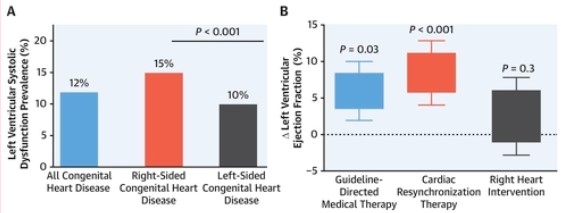
在4358名患者中,554名(12%)有LVSD,与左侧病变相比,右侧病变的LVSD患病率更高(15% vs 10%;P < 0.001)。312名(7%)患者发生了心血管事件。高LVEF与心血管事件降低独立相关(HR=0.95;95%CI:0.93-0.97)。
在544名LVSD患者中,311人接受了GDMT,48名患者接受了CRT。在接受GDMT和CRT的患者中,LVEF增加了6%(95%CI:2%-10%)和11%(95%CI:8%-14%),NT-proBNP分别减少了151pg/ml(95%CI:62-289pg/ml)和201pg/ml(95%CI:119-321pg/ml)。
综上,12%的成人CHD患者存在LVSD,在右侧病变的患者中更为常见,并与心血管事件相关。
参考文献:
Prevalence and Prognostic Implications of Left Ventricular Systolic Dysfunction in Adults With Congenital Heart Disease. J Am Coll Cardiol. 2022 Apr, 79 (14) 1356–1365
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#收缩功能障碍#
45
#JACC#
39
#患病率#
43
#ACC#
39
#先天性#
53
#左心室#
45
#功能障碍#
42
#成人先天性心脏病#
34