BMJ:社区获得性肺炎与心衰的相关性 不可不知
2017-03-24 李潇潇 环球医学
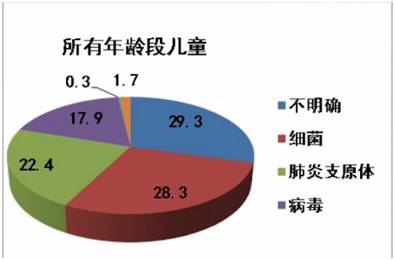
社区获得性肺炎是与高发病率和死亡率相关的常见疾病,不考虑年龄。此病是美国第七大主要死因。2017年2月,发表在《BMJ》的一项由加拿大科学家进行的10年随访的前瞻性对照研究考察了社会获得性肺炎后心衰风险。请看本期多学科讨论组临床药师各抒己见为您梳理本文看点——目的:旨在确定社区获得性肺炎对各年龄层的受影响患者和各感染严重程度患者的心衰发生率的归因风险。设计:队列研究。地点:加拿大2000~2002
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMJ#
21
#获得性#
24
#相关性#
33
感染本来就是有发心衰
54
哈哈哈
44
不错,学习了。
53
比较容易理解,肺炎导致肺组织变化。
53
好文章学习了不错!
52
#社区#
25
文章不错,值得分享
23