ALK阳性肺癌全新III期临床研究成果
2018-11-30 佚名 肿瘤资讯
欧洲肿瘤内科学会亚洲年会 (ESMO Asia 2018) 在新加坡盛大召开。主席专场(Presidential Symposium),中山大学肿瘤防治中心张力教授口头报道了亚裔ALK阳性非小细胞肺癌(NSCLC)III期ALESIA研究的主要结果。
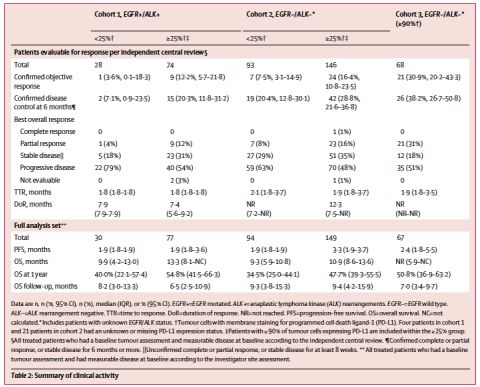
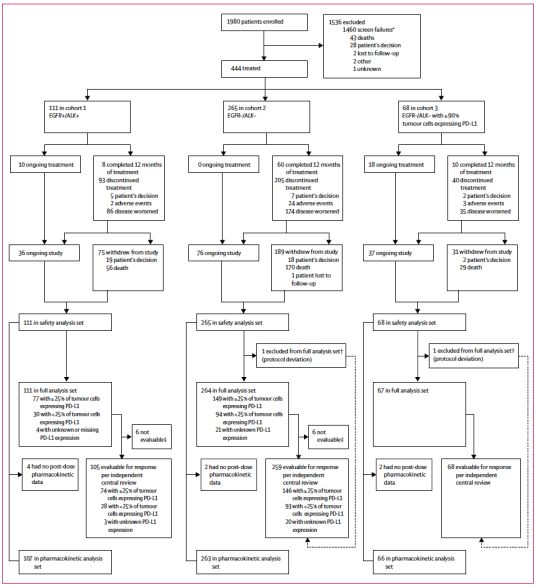
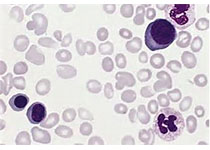
ALESIA研究由周彩存教授、张力教授担任共同PI,牵头亚洲三国多中心通力合作完成。自2016年8月3日至2017年5月16日,纳入3个亚洲国家(中国、韩国和泰国)21个中心共187名初治晚期或转移性ALK阳性NSCLC患者,以2:1随机分配进入阿来替尼治疗组(125)或克唑替尼治疗组(62)。随机后两组患者基线数据均衡。主要研究终点为研究者评估的无进展生存(PFS),次要终点包括独立评估委员会评估(IRC评估)的PFS、至CNS进展时间(IRC评估)、研究者评估的客观缓解率(ORR)、中位缓解持续时间(DOR)、总生存(OS)、安全性和耐受性。
张力教授,主任医师、博士生导师、肺癌内科首席专家,中山大学附属肿瘤医院内科主任,中山大学肺癌研究中心副主任,中山大学附属肿瘤医院国家新药(抗肿瘤药物)临床研究(GCP)中心主任、Ⅰ期病房主任,国家药品食品监督管理局(SFDA)药物评审咨询专家,澳门镜湖医院放射治疗中心顾问医生
研究者评估的PFS在克唑替尼组和阿来替尼组分别为11.1个月和尚未达到,HR 0.22(0.13-0.38);P<0.0001。IRC评估的PFS结果与研究者评估一致。PFS亚组分析结果与总体人群结果一致。研究者评估的ORR分别为 77.4%和91.2%。中位缓解持续时间分别为9.3 vs. NE,HR 0.22 (0.12 - 0.40),P<0.0001。对于基线合并可测量或不可测量颅内病灶的患者,IRC评估的CNS ORR分别为21.7%和72.7%,中位DOR分别为3.7个月和尚未达到。基线合并可测量CNS病灶的患者,CNS ORR两组分别为28.6%和94.1%。阿来替尼可以显着延缓至CNS进展风险,HR为0.14(0.06-0.30),P<0.0001;12个月的CNS进展累积发生率,克唑替尼和阿来替尼组分别为35.5%和7.3%。目前OS数据尚未成熟,但初步来看,阿来替尼显着降低患者死亡风险,HR 0.28(0.12-0.68),P=0.0027。安全性分析结果显示,两组患者发生严重 AE 比例分别为25.8%和15.2%;其中 3-5 级 AE 分别为 48.8% 和 28.8%。因AE导致治疗中止的患者比例,两组分别为9.7%和7.2%;因AE导致剂量减量的患者比例,两组分别为22.6%和24%。
总体而言,本研究为全球第三项头对头对比了阿来替尼和克唑替尼的临床试验,结果显示阿来替尼显着优于克唑替尼。此研究结果与全球ALEX研究结果一致,进一步确立了阿来替尼在ALK阳性NSCLC患者一线治疗的地位。
张力教授是中山大学肿瘤防治中心内科主任、中山大学肺癌研究中心副主任中山大学附属肿瘤医院国家新药(抗肿瘤药物)临床研究(GCP)中心主任、Ⅰ 期病房主任。长期从事肺癌的内科治疗工作及抗癌药物研究。2016 年获得国家重点研发计划 “肺癌精准治疗” 项目首席专家(2016YFC0905500),ALESIA研究亦获得该国家重点研发计划的资助。多次登上美国临床肿瘤学年会、欧洲肿瘤内科学年会及世界肺癌大会等做口头报告。近年来发表 SCI 论文 100 余篇,包括国际顶级专业杂志 Lancet, Lancet Oncology, Journal of Clinical Oncology, JAMA Oncology, JNCI 等。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#临床研究成果#
29
#ALK阳性#
30
#III期临床研究#
0
#I期临床#
24
#II期临床研究#
28
#研究成果#
22
#III#
32
#II期临床#
25
#III期#
23