NEJM:抗PD-1与抗CTLA-4一线治疗晚期黑色素瘤头对头比较,前者胜出(KEYNOTE-006研究)
2015-04-30 MedSci MedSci原创
首个比较两种免疫检查点抑制剂一线治疗晚期黑色素瘤的随机Ⅲ期试验结果日前在AACR2015会议上报告,同时,这项研究的结果已于4月19日在《新英格兰医学杂志》上在线发表。这项被称为KEYNOTE-006的试验结果显示,Pembrolizumab在各个试验终点上的表现均优于伊匹单抗。“这是第一个对两种免疫检查点抑制剂一线治疗黑色素瘤进行头对头比较的临床试验。”主要研究者、美国加利福尼亚大学洛杉矶分校J

首个比较两种免疫检查点抑制剂一线治疗晚期黑色素瘤的随机Ⅲ期试验结果日前在AACR2015会议上报告,同时,这项研究的结果已于4月19日在《新英格兰医学杂志》上在线发表。这项被称为KEYNOTE-006的试验结果显示,Pembrolizumab在各个试验终点上的表现均优于伊匹单抗。
“这是第一个对两种免疫检查点抑制剂一线治疗黑色素瘤进行头对头比较的临床试验。”主要研究者、美国加利福尼亚大学洛杉矶分校Jonsson综合癌症中心肿瘤学教授Antoni Ribas介绍该项研究时这样表示,“我们在16个国家开展了这项研究……比较了抗PD1单抗Pembrolizumab和抗CTLA-4单抗伊匹单抗。”
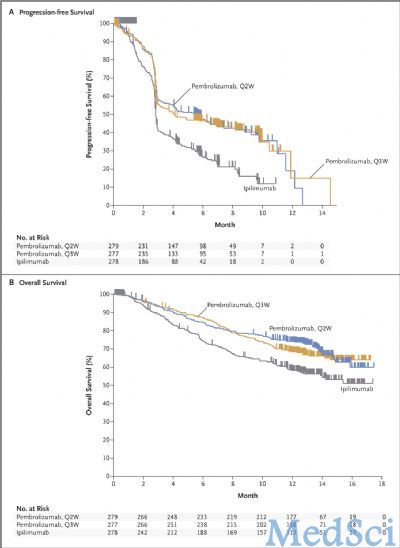
这项研究共纳入了834例转移性黑色素瘤患者,66%为初治,79%表达PD-L1。患者按1∶1∶1比例随机分为三组,分别接受10 mg/kg Pembrolizumab,每2周1次或10 mg/kg Pembrolizumab每3周1次或3 mg/kg伊匹单抗,每3周1次共4次治疗。主要终点为无进展生存(PFS)和总生存(OS)。结果显示,治疗6个月后,Pembrolizumab组的PFS为47.3%(两周方案)和46.4(三周方案),伊匹单抗组为26.5%(P<0.001)。估计的12个月OS在Pembrolizumab组分别为74.1%(两周方案)和68.4%(三周方案),而伊匹单抗组为58.2%((P值分别为0.0005和0.0036)。在总缓解率上,Pembrolizumab组也显著优于伊匹单抗组。此外,Pembrolizumab组的药物相关不良事件发生率也较伊匹单抗组低(13.3%和10.1%对比19.9%)。
Ribas教授表示,“20年前,在利用免疫系统治疗癌症这一点上,我们的思想发生了根本性的变化,而20年后的今天,我们有了确凿的证据证实这个方法能够帮助患者。”
原始出处:
Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, Daud A, Carlino MS, McNeil C, Lotem M, Larkin J, Lorigan P, Neyns B, Blank CU, Hamid O, Mateus C, Shapira-Frommer R, Kosh M, Zhou H, Ibrahim N, Ebbinghaus S, Ribas A; KEYNOTE-006 investigators. Pembrolizumab versus Ipilimumab in Advanced Melanoma.N Engl J Med. 2015 Apr 19.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#色素#
33
#KEYNOTE#
41
#头对头#
47
#CTLA-4#
35
#黑色素#
25
#黑色素#
30
相关知识不太了解
52
最好二者联合使用
138