
痛风是男性最常见的炎症性关节炎,在西方国家,至少有1%的人口会受到痛风的影响。它的特点是在关节和其他组织中形成尿酸单钠晶体。晶体触发促炎细胞因子的释放,导致炎症,导致痛风性关节炎。痛风性关节炎可发展为慢性变形和身体残疾的疾病,其发展过程为关节受损、关节破坏和持续性疼痛。痛风石是尿酸钠的结节状肿块。痛风石可以导致感染,引起疼痛,导致功能减退。当痛风石在其他部位出现时,如心脏瓣膜、腕管、喉部和脊柱,也可能导致其他并发症。痛风常因不治疗使得病情发展。本文目的是评价痛风患者痛风石的非手术治疗和手术治疗的利弊。
研究方法:我们更新了Cochrane中央对照试验注册(Central Register of Controlled Trials, Central)、MEDLINE和Embase数据库,并检索到2020年8月28日。我们使用GRADEpro软件(GRADEpro GDT)生成调查结果表。按照Cochrane的建议,这些表格提供了有关证据的确定性、干预措施的影响程度以及最重要的参与者相关结果(痛风石完全溶解的参与者数量、关节疼痛减少,研究参与者因不良事件退出的数量,总不良事件,与健康相关的生活质量,血清尿酸盐正常化和功能)。我们纳入了所有发表的随机对照试验(RCT)或对照临床试验(CCT),这些试验采用伪随机化的方法,将患者分配到需要痛风石治疗组中。虽然我们最初的检索包括了其他类型的研究,但这篇文章只包括了用于评估治疗益处的试验和伪随机对照试验,以了解痛风患者痛风石的干预措施。
主要结果:
我们在最初的评估中纳入了一项试验。我们在这次更新中增加了四个试验(1796名参与者)。第一个研究共有三组:每两周输注Pegloticase一次(双周)、Pegloticase输注与安慰剂每两周输注交替一次和输注安慰剂。两项研究观察了Lesinurad 200mg或400mg与别嘌呤醇的联用。一项试验研究了Lesinurad 200mg或400mg与非布司他联用。一项试验将80mg和120mg的非布司他+别嘌呤醇进行了比较。
由于缺乏参与者和试验人员的盲法信息,两个试验的表现和检测偏差风险都不明确。所有其他试验的偏倚风险都很低。
中度确定性证据(因不精确而降级;一项研究;79名参与者)显示:一、每两周输注Pegloticase一次(双周)组结果:①与安慰剂组相比,21/52名参与者双周使用pegloticase治疗组可以溶解痛风石,而安慰剂组为2/27,(风险比(RR) 5.45, 95%置信区间(CI) 1.38 - 21.54;与安慰剂组(41/43)相比;②接受双周pegloticase治疗组(80/85)的受试者出现不良事件的比例相似(RR 0.99, 95% CI 0.91 - 1.07)。③与安慰剂组(1/43)相比,接受双周pegloticase治疗组(15/85)的参与者因不良事件而退出比例更高(RR 7.59, 95% CI 1.04 - 55.55;因伤害而需要治疗的人数(NNTH) 7, 95% CI 4-16)。二、每月服用pegloticase治疗组结果:①与安慰剂(2/27)相比,每月服用pegloticase治疗组的参与者(11/52)显示痛风石完全消退比例更高(RR 2.86, 95% CI 0.68 - 11.97;NNTB 8, 95% CI 4至91);②与安慰剂组(41/43)相比,每月服用pegloticase组(84/84)发生不良事件的人数相似(RR 1.05, 95% CI 0.98至1.14)。③与安慰剂组(1/43)相比,每月使用pegloticase组(16/84)的更多参与者因不良事件而退出(RR 8.19, 95% CI 1.12 - 59.71;NNTH 6, 95% CI 4至14)。输液反应是最常见的原因。
中度确定性证据(2项研究;103名参与者)显示:与安慰剂加+嘌呤醇组(16/50)相比,Lesinurad 200mg+别嘌呤醇组(11/53)的靶向痛风石完全消退没有临床上的显著性差异(RR 0.40,95%CI为0.04至4.57);与安慰剂+别嘌呤醇组(16/50)相比,Lesinurad 400mg+别嘌呤醇组(12/48)临床上的完全缓解没有显著性差异(RR为0.79,95%CI为0.42至1.49),而安慰剂组与安慰剂+别嘌醇组(RR0.79,95%CI为0.42至1.49)相比,差异无显著性(RR0.40,95%CI为0.04至4.57)。
一项扩展实验研究了lesinurad 200mg或400mg与非布索坦或安慰剂联合用药(低确定性证据,因间接和不精确而降级)。在最初的研究中,受试者继续使用Lesinurad 同样的剂量。Lesinurad 400mg +非布司他可能有利于痛风石的分解;lesinurad 400 mg CONT组的43/65和lesinurad 200 mg CONT组的38/64具有痛风石溶解差异(RR 1.11, 95% CI 0.85 - 1.46)。与lesinurad 200 mg CONT组(50/64)相比,lesinurad 400 mg CONT组(57/65)发生的不良事件无差异(RR 1.12, 95% CI 0.96至1.32)。Lesinurad 400mg+非布司他可能不会导致因不良事件而停药的差异;Lesinurad 400mgCONT组中有10/65的参与者因不良事件而退出,而Lesinurad 200 mg CONT组的10/64名参与者因不良事件退出(RR 0.98,95%CI为0.44至2.20)。Lesinurad 400 mg +非布索坦没有导致平均血清尿酸(sUA)产生差异,在Lesinurad 400 mg CONT组为3 mg/dl,而在Lesinurad 200 mg CONT组为3.9 mg/dl(平均差异-0.90,95% CI -1.51至-0.29)。
在原始研究中未服用Lesinurad 的参与者被随机分组(CROSS),分别服用200mg或400mg,两者均与非布司他联合使用。由于间接和不精确而降低的低确定性证据表明,与lesinurad 200 mg (CROSS)(14/33)相比,lesinurad 400 mg (CROSS)可能导致痛风石溶解(17/34)(RR 1.18, 95% CI 0.70至1.98)。Lesinurad 400 mg联合非布司他可能不会导致不良事件的差异(Lesinurad 400 mg CROSS组为33/34,Lesinurad 200 mg CROSS组为27/33;RR 1.19, 95% CI 1.00 - 1.41)。Lesinurad 400mg联合非布司他可能没有因不良事件而停药导致的差异,Lesinurad 400mg CROSS组的停药率为5/34,而非布司他的停药率为2/33(RR 2.43, 95% CI 0.51 - 11.64)。Lesinurad 400 mg +非布司他的sUA (4.2 mg/dl, Lesinurad 400 mg CROSS)与Lesinurad 200 mg/dl (3.8 mg/dl, Lesinurad 200 mg CROSS)无差异,平均差异0.40 mg/dl, 95% CI -0.75至1.55。


表1 Pegloticase每两周(双周)与安慰剂治疗痛风的痛风石比较

表2 Lesinurad200mg+别嘌呤醇与安慰剂+别嘌呤醇治疗痛风效果的比较
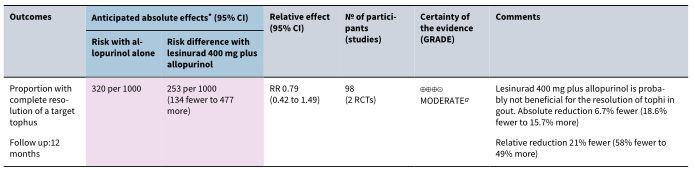
表3 Lesinurad400mg+别嘌呤醇与安慰剂+别嘌呤醇治疗痛风效果的比较


表4 Lesinurad 400mg+非布司他与Lesinurad 200mg+非布司他治疗痛风效果的比较
结论:中度确定的证据表明,pegloticase可能有利于痛风中的痛风石溶解。尽管与安慰剂相比,pegloticase组的不良事件差异不大,且由于不良事件,pegloticase组有更多的患者停药。Lesinurad 400mg +非布司他与Lesinurad 200mg +非布司他相比,有利于痛风石的溶解,两组之间的不良事件没有差异。我们无法确定lesinurad+非布索坦是否比安慰剂更有效。Lesinurad(400mg或200mg)+别嘌呤醇可能对痛风石溶解无益,两组之间的不良事件没有差异。痛风患者痛风石干预治疗的随机对照试验是必要的,仍缺乏试验数据。
原文出处:
Sriranganathan MK, Vinik O, Pardo Pardo J,et al.Interventions for tophi in gout.Cochrane Database Syst Rev 2021 Aug 11;8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#相关研究#
55
赞
36
#治疗方案#
48
学习了
44
感谢分享
47
#痛风石#
38
#CDS#
44
痛风结石的治疗学习了,非常实用
51
痛风是男性最常见的炎症性关节炎,
58
学习一下
49