Stroke:自发性脑内出血的形成机制——基于解剖学的研究
2022-09-10 MedSci原创 MedSci原创
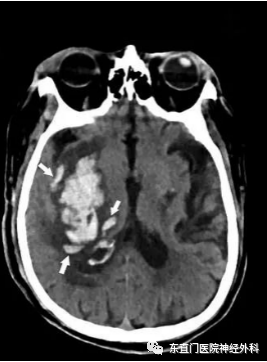
形成的基底节脑内血肿最初在血管周围空间扩散,使分支与神经组织分离,并引起继发性出血。
尽管在了解各种风险和预后因素方面取得了进展,但自发性脑内出血的发病率和死亡率都非常高,而治疗主要是支持性的。由于临床数据不足和缺乏合适的动物模型,对初始血肿扩张的病理生理学的理解是有限的。
近期。来自波兰华沙大学的学者给40个基底神经节的解剖标本注射造影剂,用微型计算机断层扫描器进行扫描,并分析放射学研究、直接和组织学检查的结果。相关成果发表在Stroke杂志上。
在9个病例中,微型CT和组织学检查显示造影剂外渗模仿了脑内血肿。人工血肿沿破裂的穿孔器及其分支在血管周围空间向近端和远端扩散,并使分支与邻近的神经组织分离,导致组织的破坏和继发外渗。此外,一些造影剂外渗跳到未破裂的穿孔器的血管周围空间,形成进一步的外渗部位,加剧了人工血肿的扩大。没有任何人工血肿向蛛网膜下层延伸。

研究人员推测,形成的基底节脑内血肿最初在血管周围空间扩散,使分支与神经组织分离,并引起继发性出血。
它也可以跳到附近穿孔器的血管周围空间。所提出的血肿启动和形成机制解释了神经组织的损伤程度、时间和空间的增长变化、继发性出血点的产生以及手术干预的有限效用。该模型是可重复的,人工血肿的范围很容易控制,穿孔动脉的破裂部位可以确定,而且除了微型计算机断层扫描仪外,模型的准备不需要专门的、昂贵的设备。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#脑内出血#
46
#自发性脑内出血#
35
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
42
#自发性#
39
#解剖学#
65