JAMA Ophthalmol:MIOCTA用于儿童视网膜血管病
2017-04-10 MedSci MedSci原创
MIOCTA用于儿童视网膜血管病的首次报道,该技术有望应用于多种情况下的非侵入性视网膜血管检查。
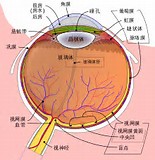
术中的光学相干断层成像(OCT)是玻璃体视网膜手术中临床决策的重要辅助手段,OCT血管造影法(OCTA) 为视网膜疾病的临床评价提供了新的见解。至目前为止,这两种技术还没有在视网膜血管疾病手术中联合使用。近日研究人员在视网膜血管病儿童尝试使用显微镜集成,扫频源光学相干断层成像血管造影法(MIOCTA)。
研究在儿童眼科患者中进行,主要目的是研究MIOCTA和荧光素眼底血管造影的对比。
在2例儿童视网膜血管病中,相比于荧光素眼底血管造影,MIOCTA显示更为细致的血管情况。MIOCTA系统可视化视网膜周边视网膜血管的微小病变,而这些病变会被遮蔽在荧光素眼底血管造影的荧光素染色下。
这是MIOCTA用于儿童视网膜血管病的首次报道,该技术有望应用于多种情况下的非侵入性视网膜血管检查。
原文出处:
Xi Chen et al. Microscope-Integrated Optical Coherence Tomography Angiography in the Operating Room in Young Children With Retinal Vascular Disease. JAMA Ophthalmol. 2017-4-6.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#OCT#
0
#CTA#
24
#血管病#
23
#视网膜#
31
#THA#
23