FDA黑框警告!氟喹诺酮类药品需慎用!
2016-07-28 佚名 医学界药学频道
2016年7月26日,FDA批准更新氟喹诺酮类药物(包括口服制剂和注射液)的药品标签。氟喹诺酮类药物全身用药时致残性和潜在的永久性严重不良反应可同时发生,这些不良反应累及肌腱、肌肉、关节、神经和中枢神经系统,因此FDA不但修订了黑框警告,特别强调用药的安全性问题,此外FDA还增加了新的警告,且同步更新了药品标签中用药指南等其他内容。此次FDA更新了氟喹诺酮类药品标签中的黑框警告,并增加了新的警告,
2016年7月26日,FDA批准更新氟喹诺酮类药物(包括口服制剂和注射液)的药品标签。
氟喹诺酮类药物全身用药时致残性和潜在的永久性严重不良反应可同时发生,这些不良反应累及肌腱、肌肉、关节、神经和中枢神经系统,因此FDA不但修订了黑框警告,特别强调用药的安全性问题,此外FDA还增加了新的警告,且同步更新了药品标签中用药指南等其他内容。
此次FDA更新了氟喹诺酮类药品标签中的黑框警告,并增加了新的警告,还修订了患者用药指南等内容。具体内容如下:
黑框警告
原有的黑框警告:氟喹诺酮类药物可能引起肌腱炎、肌腱断裂和重症肌无力病情恶化的警告标签。
新增黑框警告:氟喹诺酮类药物可能致残及并发多种永久性严重不良反应。
警告及注意事项:
原有警告:氟喹诺酮类药物可能引起肌腱炎、肌腱断裂和重症肌无力病情恶化、外周神经病变风险及中枢神经系统不良反应,还包括一些心脏、皮肤及过敏反应等严重不良反应。
新增(进一步加强警告):氟喹诺酮类药物全身用药时致残性和潜在的永久性严重不良反应可同时发生,这些不良反应包括肌腱炎、肌腱断裂、中枢神经系统相关反应、重症肌无力恶化、外周神经系统病变、QT间期延长、尖端扭转型室速及光毒性。这些不良反应可发生在用药后几小时内至几周内,且几种不良反应可能会同时发生。
适应证和用法:
增加了新的限制使用说明:急性细菌性鼻窦炎(ABS)、慢性支气管炎的急性细菌感染性恶化(ABECB)、单纯性尿路感染患者使用氟喹诺酮类抗菌药品治疗引发相关严重不良反应的风险通常大于效益,因此针对上述疾病,氟喹诺酮类药品应该仅用于那些没有其他方案可供选择的患者。
此外氟喹诺酮类药物可用于治疗炭疽病、瘟疫、细菌性肺炎等严重细菌感染患者,获益大于风险。
用药指南:
患者用药指南中新增要求:在给患者开具喹诺酮类处方时,应让每位患者都了解具体的药物安全性问题。
氟喹诺酮类药物不良反应
氟喹诺酮类全身性使用的严重不良反应:
肌肉、骨骼及外周神经系统 | 中枢神经系统 | 其它器官及系统 |
肌腱炎 | 焦虑 | 重症肌无力的恶化 |
肌腱断裂 | 抑郁 | 皮疹 |
麻木、刺痛、手臂及腿部刺痛感“针样刺痛” | 幻觉 | 晒伤(光毒性) |
肌无力 | 自杀倾向 | 心脏搏动异常、快速强烈 |
肌痛 | 困惑 | 严重腹泻 |
关节痛 |
氟喹诺酮类药物的常见不良反应:恶心、腹泻、头痛、头晕、晕眩或入睡困难。
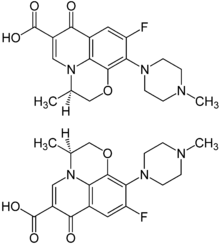
目前FDA批准的全身性使用的氟喹诺酮类药物
莫西沙星
环丙沙星
环丙沙星缓释剂
吉米沙星
左氧氟沙星
氧氟沙星
FDA建议
如果患者服用喹诺酮类药物,一旦出现任何严重不良反应及相关症状,如肌腱、关节、肌肉疼痛,针样刺痛或刺痛感,混乱和幻觉,应及时告诉医务人员。医务人员应立即对出现严重不良反应的患者停药,并选择非氟喹诺酮类抗菌药进行后续治疗。FDA同时希望患者和医务人员积极上报相关药物不良反应。FDA表示将会继续跟进喹诺酮类药物的安全问题,并及时更新最新消息。
附:FDA曾经发布过的氟喹诺酮类药物安全信息通报
2008年7月,FDA要求氟喹诺酮类抗生素生产者增加关于药物可能引起肌腱炎和肌腱断裂事件的黑框警告。对于老年人、肾、心、肺脏移植者或者同时应用激素治疗的人来说,应用氟喹诺酮更容易发生肌腱炎或肌腱断裂。
2013年8月,FDA要求更新全身应用的喹诺酮类药物的使用说明书及相关用药指导,以便更好地提醒这类药物可能导致严重外周神经病变。外周神经病变的症状包括上下肢的疼痛、烧灼感、麻木、物力或者任何深浅感觉的改变。
2016年5月,FDA发布了一项药物安全性通知,严格限制氟喹诺酮类抗菌药用于鼻窦炎、支气管炎和非复杂性泌尿道感染患者,警告其可能致残甚至并发多种永久性不良反应。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#喹诺酮#
36
有用
0
#氟喹诺酮#
31
引起重视,多观察,及时与病患沟通,按需调整药物
56
继续学习
56
继续关注
68
哦
81
临床上遇到过这样的先例!
34
!!!!!!!
41