Heart:白细胞介素-6抑制剂对心肌梗死患者冠脉微血管内皮功能的有何影响?
2017-04-22 xing.T MedSci原创
由此可见,在住院期间或6个月后,托珠单抗治疗不会影响CFR。托珠单抗会增加住院期间VCAM-1的水平,但这并不与这些患者CFR降低相关。
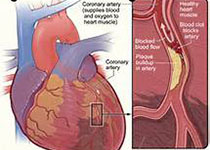
白细胞介素-6(IL-6)是急性冠脉综合征炎症和内皮细胞激活的驱动因子。近日,在心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员评估了IL-6受体拮抗剂托珠单抗对非ST段抬高型心肌梗死(NSTEMI)患者冠脉微血管功能及通过冠脉血流储备(CFR)测定的内皮功能紊乱和内皮细胞活化标志物的影响。
本研究为一个二中心、双盲、随机、安慰剂对照、旨在评估单剂量托珠单抗对NSTEMI疗效的试验的一个部分。研究人员对117例患者的内皮细胞活化标志物(血管细胞粘附分子(VCAM)-1、细胞间黏附分子-1和von Willebrand因子)进行了评估。研究人员将42例这样患者,其中的20例分配至安慰剂组,另外22例分配至托珠单抗治疗组,研究人员们测量了CFR。在第1天至第3天期间的7个连续时间点获取了血液样本。在住院期间和6个月后,研究人员采用经胸超声心动图测定了患者CFR。
住院期间,采用托珠单抗治疗没有影响CFR(托珠单抗:3.4±0.8 vs. 安慰剂:3.3±1.2,P=0.80)。两组患者在6个月后CFR明显改善。在托珠单抗组患者对于VCAM-1有显著较高的曲线下面积(托珠单抗组和安慰剂组的中位数分别为622 vs. 609 毫微克/毫升/小时,P=0.003)。在安慰剂组VCAM-1和CFR之间呈负相关(住院期间r=-0.74,P<0.01,6个月后:R=-0.59,P<0.01),但在托珠单抗组并不是(住院期间:r=0.20,P=0.37,6个月后:r=0.28,P=0.20)。
由此可见,在住院期间或6个月后,托珠单抗治疗不会影响CFR。托珠单抗会增加住院期间VCAM-1的水平,但这并不与这些患者CFR降低相关。
原始出处:
Espen Holte,et al. Effect of interleukin-6 inhibition on coronary microvascular and endothelial function in myocardial infarction. Heart. 2017. http://dx.doi.org/10.1136/heartjnl-2016-310875
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血管内皮功能#
39
#抑制剂#
30
#ART#
30
#微血管#
22
#内皮功能#
44
#HEART#
26
#白细胞介素#
47