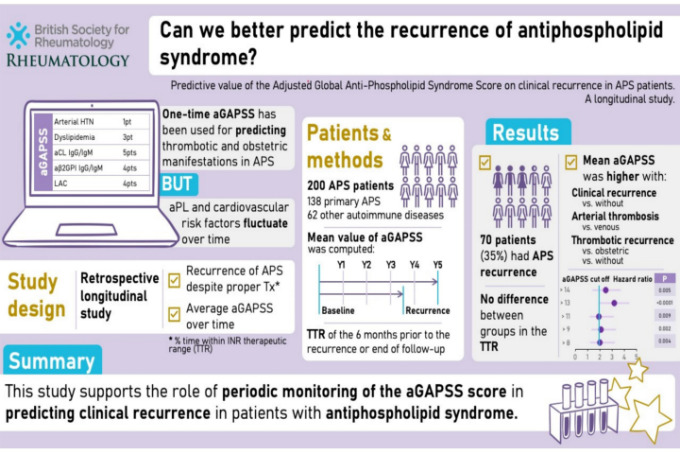
Rheumatology:抗磷脂综合征患者经校正的整体APS评分对临床复发的预测价值,一项纵向研究
2022-08-28 紫菀款冬 MedSci原创
通过一项回顾性纵向研究,评估平均校正后的整体APS总分(aGAPSS)对抗磷脂综合征(APS)患者临床表现复发的影响。
目的:通过一项回顾性纵向研究,评估平均校正后的整体APS总分(aGAPSS)对抗磷脂综合征(APS)患者临床表现复发的影响。

方法:该研究包括200例APS患者。在基线和每年的基础上计算每个患者的aGAPSS,最多6年(至少3年),或在经历临床复发的患者发生临床事件之前。并计算每个患者的平均得分。
在服用维生素K拮抗剂(VKA)的患者中,计算在治疗范围内所用时间的百分比(TTR)。进行Cox回归分析以确定与临床复发相关性最强的aGAPSS的截止值。
结果:临床复发患者的平均aGAPSS值高于未复发患者[8.81(95%CI 7.53-10.08)vs 6.38(95%CI 5.64-7.12),p =0.001]。
血栓复发患者的平均aGAPSS值高于流产复发患者[9.48(95%CI 14-10.82)vs 4.25(95%CI 0.85-7.65),p = 0.006]。
动脉血栓患者的平均aGAPSS值高于静脉血栓患者[10.66(S.D. 5.48)vs 6.63(S.D. 4.42),p = 0.01]。
在多变量分析中,aGAPSS值>13分与最高复发风险相关[HR = 3.25(95%CI 1.93-5.45,p < 0.0001]。血栓复发患者与未复发患者的TTR无统计学差异。
结论:该研究数据支持定期(每年)监测aGAPSS评分在预测APS患者临床复发中的作用。
文献来源:
Barilaro G, Esteves A, Della Rocca C, et al. Predictive value of the Adjusted Global Anti-Phospholipid Syndrome Score on clinical recurrence in APS patients: A longitudinal study [published online ahead of print, 2022 Aug 23]. Rheumatology (Oxford). 2022;keac485. doi:10.1093/rheumatology/keac485
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Rheumatology#
56
#纵向研究#
47
#综合征#
52
#APS#
63
#预测价值#
49