NEJM:转移性鳞状非小细胞肺癌一线治疗 免疫治疗+化疗生存期更长
2018-12-27 贾朝娟 环球医学
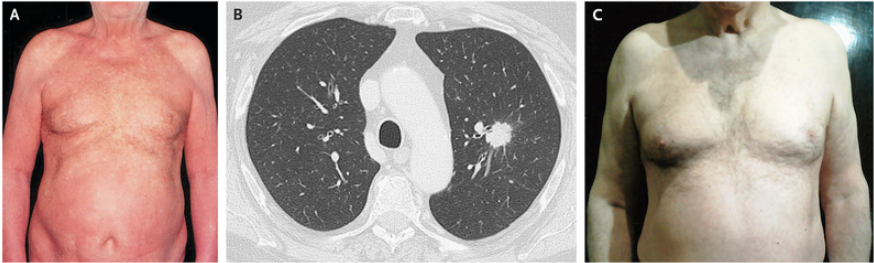
继肿瘤靶向治疗之后,近几年免疫治疗大放异彩。对于转移性鳞状非小细胞肺癌(NSCLC),帕博利珠单抗(对于肿瘤细胞表达程序死亡配体1(PD-L1)≥50%的患者)几乎已成为与化疗齐驾并驱的一线治疗。2018年11月,发表在权威杂志《N Engl J Med》的一项研究再次显示,对于转移性鳞状NSCLC患者,与单纯化疗相比,帕博利珠单抗联合化疗一线治疗可带来更多生存获益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非小细胞#
34
#转移性鳞状非小细胞肺癌#
31
#生存期#
27
#转移性#
37
学习了很有用不错
0
热门
47