溶栓后出血转化怎么办?评估、用药,专家整理好了
2022-04-12 网络 网络
溶栓后出血转化一直以来都是临床的棘手问题,很多临床医生在溶栓患者发生出血后,都会变得特别谨慎,担心又再一次出血,便不再轻易进行溶栓治疗,对于这种棘手的情况该如何处置?
溶栓后出血转化一直以来都是临床的棘手问题,很多临床医生在溶栓患者发生出血后,都会变得特别谨慎,担心又再一次出血,便不再轻易进行溶栓治疗,对于这种棘手的情况该如何处置?
在中国卒中学会第七届学术年会(CSA&TISC 2021)上,来自华中科技大学同济医学院附属协和医院的胡波教授为我们带来了题名《伴有“出血转化”卒中患者的评估及抗栓选择》讲座,内容包含出血转化的概念、分类、诊断、评估、治疗等,让我们一起来学习吧!
出血转化的概念
1990年开始,Pessin根据出血部位将其分型为:梗死后出血(H1)和脑实质出血(PH),依据CT影像学表现,每型又分为1和2两个亚型。
1994年,Levy在静脉溶栓的研究中首次使用了“症状性颅内出血”的概念和定义,将急性脑梗塞再通治疗后的脑出血与临床症状联系起来。
出血转化的分类
(一)其临床分类主要是依据几个脑血管相关的研究,包括:
①NINDS研究:在1995年,由美国国立神经病学与卒中研究所开展,纳入312名0-3小时发病的卒中患者;
②ECASS II研究:1998年欧洲协作性卒中研究,纳入407名发病0-6h卒中患者;
③SIST-MOST研究:2007年欧洲卒中安全监测研究,纳入6483例发病0-3小时发病的卒中患者;
④ECASS Ⅲ研究:2008年欧洲入选821例18-80岁的急诊梗死患者,溶栓时间窗为3-4.5h;
⑤IST-3研究:2012年第三次国际卒中研究,3035名发病0-6h卒中患者。
根据以上这些研究,将出血转化分为了症状性颅内出血(Symptomatic ICH,sICH)和非症状性颅内出血(Asymptomatic ICH,aICH)(具体分类见图1)。
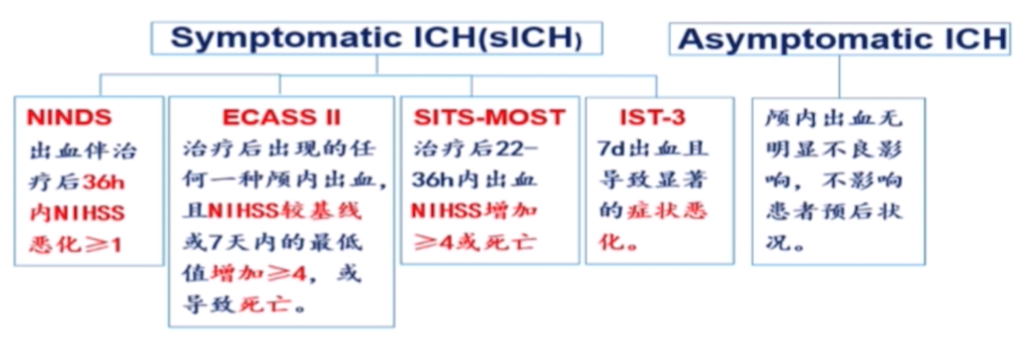
图1出血转化临床分类
(二)出血转化影像学分类
根据ECASS研究,又将出血转化进行了影像学分类(见图2):
①HI-1:沿着梗死灶边缘小的斑点状密度增高的出血点;
②HI-2:梗死灶内较大的融合的出血点,无占位效应;
③PH-1:血肿体积不大于梗死区域的30%,伴有轻微的占位效应;
④PH-2:血肿体积不大于梗死区域的30%,伴有明显的占位效应。
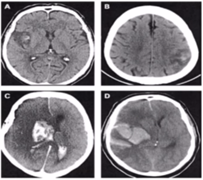
图2出血转化影像学分类
HI-1(A);HI-2(B);PH-1(C);PH-2(D)
(三)血管再通脑出血分类
2015年,脑梗死血管再通治疗后的脑出血海德堡分型(HBC),依据影像学检查的分型:
①出血转化(1a、1b、1c);
②局限于梗死区域的脑实质出血;
③梗死区外脑实质的出血或颅内-颅外出血三型(3a、3b、3c、3d)。
(四)溶栓后出血的时间一般是在什么时候呢?
溶栓后继发性颅内出血多发生在溶栓治疗后4h内;
ECASS III研究显示SICH多发生在36h内,36h后溶栓继发性出血可能性极低;
自发性出血转化发生率为5%。
诊断出血转化的7个步骤
1、治疗后48h复查影像学,根据临床脑出血状况复查影像学;
2、影像学判断由独立人员采用盲法判断;
3、脑出血按照解剖部位进行描述;
4、区分症状性脑出血(sICH)还是无症状性脑出血(aICH);
5、确定临床症状恶化和影像学相关性,分为:确定、很可能、可能的、不可能;
6、其中“确定”和“很可能”报告为sICH,“可能”或“不可能”报告为aICH;
7、判定脑出血与干预治疗之间的相关性:静脉或动脉溶栓后24h内发生的;脑出血发生在血管内治疗脑区;造影相关的并发症。其中相关性也分为:确定的、很可能的、可能的、不可能四种。
静脉溶栓后的出血转后对预后的影响
(一)症状性出血转化(sICH)
NINDS:死亡率为45%;
PH-2:ECASS研究显示对患者长期预后不利;
PH-1:ECASS研究显示仅影响近期预后;
HT-1:ECASSII研究显示良好结局。
(二)无症状性出血转化(aICH)
荟萃NINDS、ECASSII、Atiantis A and B Trials显示3个月预后无影响。
静脉溶栓后出血转化的危险因素有哪些呢?
荟萃分析纳入55项静脉溶栓危险因素研究(n=65264)显示:年龄、高NIHSS评分、高血糖是出血转化的独立危险因素;
荟萃分析纳入中国人的14项静脉溶栓危险因素研究(n=2548)显示:年龄、房颤、卒中病史、服用抗血小板药物病史、较高的NIHSS评分、血压、血糖水平是溶栓后出血转化的独立危险因素;
荟萃分析纳入11项研究(n=7194)显示:脑白质疏松是sICH独立预测因子;
荟萃分析纳入8个研究(n=2601)显示:脑微出血灶超过10个对出血转化可能会有影响(总结见图3)。
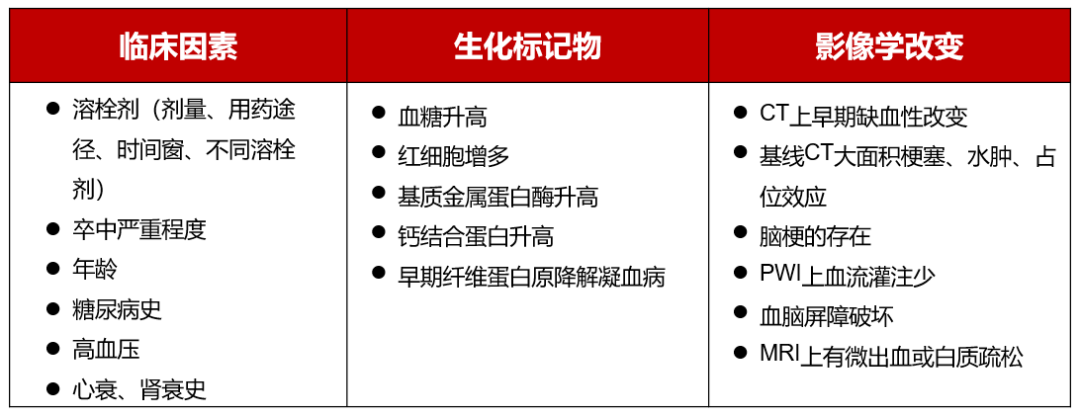
图3 rt-PA溶栓后出血转化的危险因素
溶栓后出血转化的预测评分
溶栓后出血(HAT)评分是一种实用、快速且易于操作的评分标准:基线血压、NIHSS评分、CT扫描梗塞面积,可以对溶栓后脑出血进行合理的风险分层;
SEDAN评分(0~6分):基线血糖、早期入院时CT扫描、年龄、入院时NIHSS评分(≥10分,得分=1)、梗塞体征(是=1分)、(高)密度脑动脉征(是=1)。推导队列中sICH的绝对风险分别为0~5的评分,对应风险分别为1.4%、2.9%、8.5%、12.2%、21.7%和33.3%。
如何预防溶栓后脑出血转化?
血液学检查:凝血功能、血常规、血小板计数、肝功能、肾功能、血糖;
病情严重程度评价:NIHSS评分>25分或昏迷;
剂量不能超过0.9mg/kg;
称体重,准确计算所需剂量;
溶栓后24h内不用抗血小板药物和抗凝药物。
选择rt-PA作为溶栓药物:相对纤溶特异性:半衰期短、代谢快;多个RCT广泛证实,安全可靠;
把握治疗时间窗:4.5h(越早越好);
控制血压:SBP>185mmHg,DBP>110mmHg为禁忌;
控制高血糖:血糖<2.7mmol/l或>22.2mmol/l为禁忌。
溶栓后脑出血转化的发生机制
与rt-PA本身结构是有关系的:rt-PA具有酶活性,高效激活血栓纤溶酶原为纤溶酶,发挥溶栓功能;溶栓后rt-PA滞留血脑屏障(BBB)及其多靶点作用,增加溶栓后出血转化风险;
再灌注损伤:脑梗死出血转化发生率与血管再通时间呈显著正相关;缺血时间延长引起一系列复杂瀑布级联反应,破坏BBB,使血液有害成分渗入脑组织,形成恶性循环;
BBB通透性增加:动物研究证实rt-PA可激活PDGF-CC,损害BBB完整性,导致出血转化。
溶栓后发生出血转化的机制,可能为我们研究溶栓后出血转化的干预方面,提供相应的靶点,例如:聚焦rt-PA加重血脑屏障破坏机制、MMP抑制剂、自由基清除剂、炎症抑制剂等。
溶栓出血转后的抗栓治疗怎么选择呢?
中外指南一致推荐急性期多数患者首选含阿司匹林的抗板治疗;
国内外指南对高危TIA和轻型缺血性卒中早期推荐双联抗板治疗;
阿司匹林是国内外指南长期抗栓方案的共同推荐;
国内外指南/共识推荐脑出血患者,如有抗栓指征,应及时恢复抗栓治疗,时机需个体化;
冠心病双联抗血小板治疗中国专家共识(2021年):接受双抗的高出血风险患者应继续使用或恢复阿司匹林治疗;
当发生消化道出血后,需根据再出血风险,决定继续使用原抗板方案,或继续服用/及时恢复服用阿司匹林。
来源:医学界神经病学频道
汇报专家:胡波教授 华中科技大学同济医学院附属协和医院
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








非常实用,多谢!
0
打卡打卡的
37
打卡打卡,。
34
学习啦,,
37
学习了
47