Neurol Neuroimmunol Neuroinflamm: OCT检查视网膜层厚度有助于早期识别多发性硬化患者认知障碍风险
2021-05-29 MedSci原创 MedSci原创
OCT可能提供机会,以一种成本效益和可行的方式尽早识别有CI风险的MS患者。这样,OCT结果可能推动在适当的时候开始实施广泛的神经心理评估和定期监测评估。

对于多发性硬化症(MS)患者,认知障碍(CI)可能是该疾病的突出症状,甚至在早期阶段。尽管需要定期进行神经心理评估以尽早确定CI,但适当的检查尚未纳入既定的临床护理监测标准。
光学相干断层扫描(OCT)测量的视网膜层厚度(RLT)被认为是多发性硬化(MS)神经退行性变的一种非侵入性、经济有效的标志物。Sharon Jean Baetge等研究多发性硬化患者RLT与国际MS医学认知评估(BICAMS)中的认知能力的关系,以及轻度到中度临床缺陷的门诊患者的注意和执行功能测试,以探讨OCT指向CI的潜力。该研究结果发表在Neurol Neuroimmunol Neuroinflamm杂志。
该研究数据来源于一项干预性研究的基线检查。通过广义估计方程(GEE)分析来调查RLT与认知表现的关系,以及它作为MS患者认知状态指标的潜力。
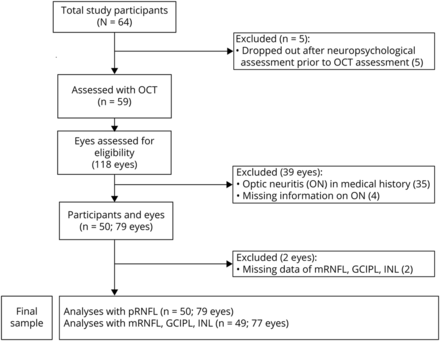
上图显示了排除、退出和最终样本情况。64名参与者,59名接受OCT检查。经质量控制、剔除缺失数据、既往ON病史或缺失ON信息的数据后,pRNFL数据79只眼,mRNFL数据77只眼,GCIPL数据77只眼,INL数据77只眼。“n”为参与研究的人数。括号中的数字显示眼睛的数量。GCIPL =黄斑神经节细胞内网状层;INL =内核层;mRNFL =黄斑视网膜神经纤维层;光学相干层析;ON =视神经炎; pRNFL视网膜乳头周围神经纤维层。
在这项横断面研究中,至少有轻度认知损伤迹象的患者接受了OCT、国际MS认知评估和注意力和执行功能测试(Trail Making Test [TMT] A和B)的检查。这些因素的关联采用GEE模型进行调查,控制人口统计学和疾病相关因素,并进行多项测试校正。
共64例患者进入研究。在最终的样本中(n = 50 [n = 14由于缺失数据或退出而被排除];44例复发缓解型MS和6例继发性进展型MS,平均扩展残疾状态量表评分= 2.59 [SD = 1.17],疾病持续时间[中位数]= 7.34[四分位数范围= 12.1],有36.0%认知功能受损。黄斑视网膜神经纤维层的RLT与TMT-B的表现相关(β =−0.259)。对RLT的上分位数和下分位数的分析进一步揭示了黄斑神经节细胞内网状层和TMT-B与言语短期记忆和学习的关系。

pRNFL、mRNFL、GCIPL和TMT-B的认知表现之间相关关系散点图

上图描绘了每个RLT极端组的认知表现的原始分数。(A) TMT-B)、VLMT和Brief、BVMT-R的认知表现分为黄斑神经节细胞内丛状层(mGCIPL)视网膜层厚度(RLT)的低三分位数和高三分位数。(B)TMT-B的认知表现分为黄斑神经节细胞内丛状层(mGCIPL)视网膜层厚度(RLT)的低三分位数和高三分位数(所有分析包括TMT-B,剔除2个离群值)。*认知测验的原始得分在RLT的低和高分位数之间存在显著差异。
在MS患者中,在较低的疾病阶段,RLT特别与认知灵活性相关,促进OCT作为一个潜在的标志物,提倡进一步广泛的神经心理学检查。
总之,RLT和BICAMS在轻度至中度临床缺陷患者中似乎是互补的方法,因为在纠正多重检测时,SDMT和BVMT-R与RLT没有相关性。然而,由于检测到mRNFL和GCIPL的厚度与认知灵活性的关系,当显示异常时,mRNFL和GCIPL的厚度可能成为进一步广泛的神经心理测试的标志。由于神经心理评估(如BICAMS)仍未普遍应用于MS患者的诊断过程和监测,OCT可能提供机会,以一种成本效益和可行的方式尽早识别有CI风险的MS患者。这样,OCT结果可能推动在适当的时候开始实施广泛的神经心理评估和定期监测评估。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#多发性#
51
学习了
49
#OCT#
49
#LAM#
46
#Neurol#
37
#视网膜#
42
#NFL#
33
#CT检查#
39