JCC:细菌和真菌谱可以作为炎症性肠病患者对于英夫利昔单抗药物反应的标志物
2020-12-16 MedSci原创 MedSci原创
在过去的20年中,越来越多的研究表明,肠道菌群的组成与改变在炎症性肠病(IBD)的发病机制中起着关键作用。
在过去的20年中,越来越多的研究表明,肠道菌群的组成与改变在炎症性肠病(IBD)的发病机制中起着关键作用。与健康人相比,IBD患者的肠道微生物多样性明显降低,IBD患者中具有抗炎能力的细菌,例如产短链脂肪酸(SCFA)的梭状芽胞杆菌类的细菌数量减少,真菌数量出现异常等等都在炎症性肠病的发生发展中扮演着重要作用。

英夫利昔单抗(IFX)是一种TNF-α阻滞剂,尽管三分之一的患者最后会对治疗出现无反应,但它已成功用于治疗IBD患者。但是目前没有可靠的生物标志物可用于预测IFX反应情况,因此,本项研究的目的是调查IFX治疗期间的IBD患者的粪便细菌和真菌群落组成差异,并为IBD患者寻找IFX治疗反应的预测因子。
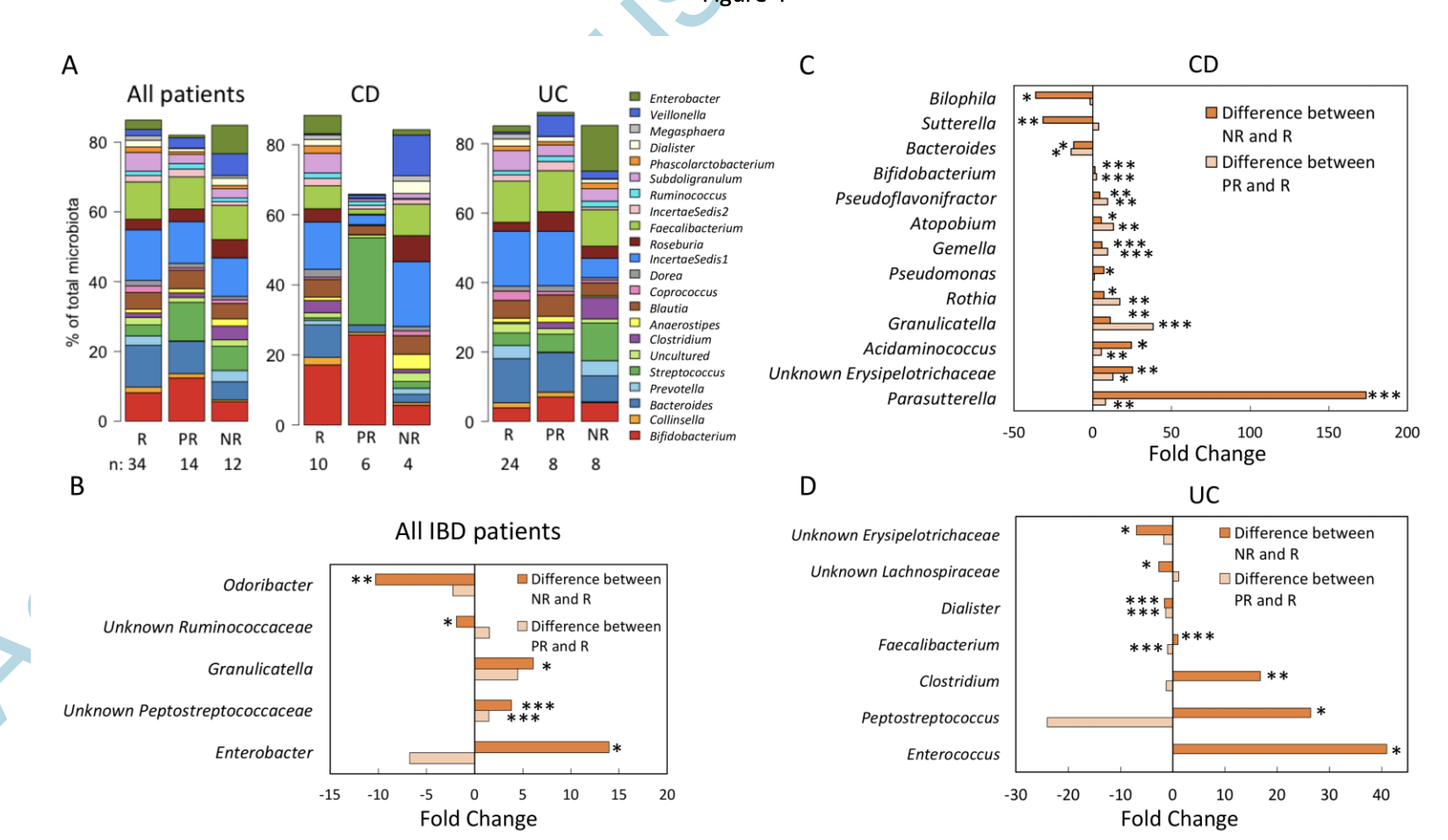
研究人员对72名IBD患者(25 CD和47 UC)进行了IFX治疗,并随访了一年或直到IFX治疗中断。在确定IFX治疗前分别针对患者体内的细菌16S rRNA基因和真菌ITS 1区的扩增子测序,然后在治疗开始后两周,六周,十二周和一年的粪便样品中的微生物群谱进行再次测序。对IFX的反应是通过结肠镜检查和开始后十二周的临床评估来进行判断的。
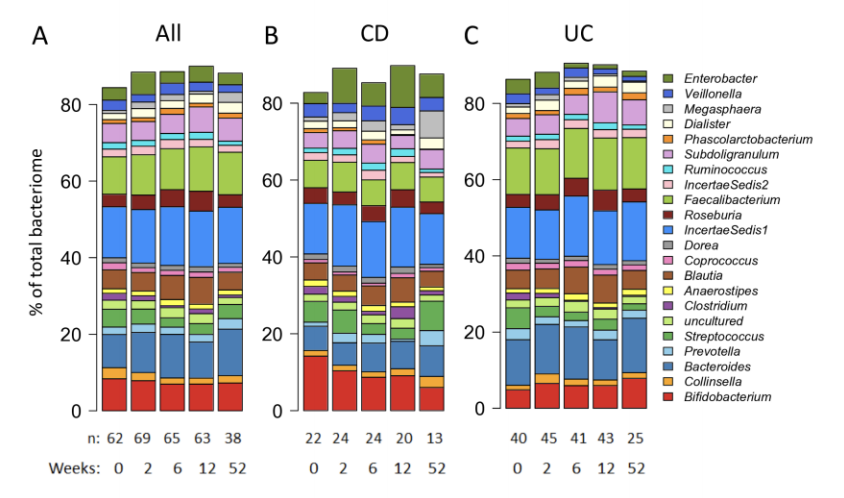
研究结果显示在开始IFX治疗之前,响应组与未响应组之间的粪便细菌和真菌特征均存在显着差异。与响应者相比,无响应者的短链脂肪酸生产者(尤其是梭菌属)的丰度较低,而促炎性细菌和真菌(例如念珠菌属)的丰度较高。由此,研究者们认为细菌类群可预测CD和UC患者的反应(曲线下面积> 0.8)。
原始出处:
Rebecka Ventin-Holmberg. Et al. Bacterial and fungal profiles as markers of infliximab drug response in inflammatory bowel disease. Journal of Crohn's and Colitis.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#药物反应#
51
#标志物#
38
#单抗药#
41
#真菌#
43
#炎症性#
44
#炎症性肠病患者#
30
学习受用
94