J Am Soc Nephrol:HDL胆固醇的流出能力不能预测血透患者心血管发生的风险
2016-10-09 phylis 译 MedSci原创
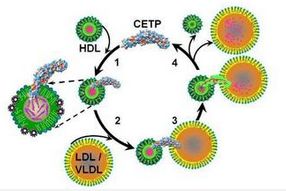
高密度脂蛋白(HDL)的保护作用主要是由胆固醇流出能力决定的,这表明肾功能正常人群中HDL与动脉粥样硬化性心血管疾病是负相关的。终末期肾病患者ESRD有异常高的心血管风险,这些风险不能完全由传统的危险因素解释。在这里,对参与德国糖尿病透析研究中的1147例血液透析的2型糖尿病患者进行post-hoc分析,研究者调查高密度脂蛋白胆固醇流出能力是否能预测心血管风险。通过孵化人巨噬细胞消耗血清apoB量
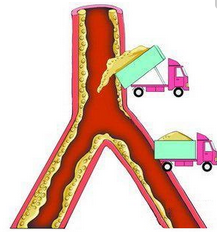
高密度脂蛋白(HDL)的保护作用主要是由胆固醇流出能力决定的,这表明肾功能正常人群中HDL与动脉粥样硬化性心血管疾病是负相关的。终末期肾病患者ESRD有异常高的心血管风险,这些风险不能完全由传统的危险因素解释。
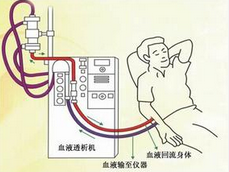
在这里,对参与德国糖尿病透析研究中的1147例血液透析的2型糖尿病患者进行post-hoc分析,研究者调查高密度脂蛋白胆固醇流出能力是否能预测心血管风险。通过孵化人巨噬细胞消耗血清apoB量化外排能力。
在平均4.1年的随访中,423的患者达到主要复合终点(心血管死亡、非致死性心肌梗死和脑卒中的复合),410患者出现心脏事件,561例死亡。值得注意的是,在Cox回归分析中,研究者没有发现流出能力与主要复合终点(HR,0.96;95% CI,0.88,1.06;P = 0.42),心脏事件(HR,0.92;95% CI,0.83-1.02;P = 0.11),及全因死亡率(HR,0.96;95% CI,0.88到1.05;P = 0.39)没有相关性。
总之,高密度脂蛋白胆固醇流出能力不是血液透析的糖尿病患者心血管危险因素的预测因子。
原始出处:
Kopecky C, Ebtehaj S, etal. HDL Cholesterol Efflux Does Not Predict Cardiovascular Risk in Hemodialysis Patients. J Am Soc Nephrol. 2016 Sep 9.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血管发生#
28
继续关注中
47
好文章,受益
58
#HDL#
24
#HDL胆固醇#
35
#血透#
29