Int J Cardiol:LDL-C和非HDL-C水平与缺血性卒中风险增加显著相关
2016-07-20 phylis 译 MedSci原创
背景:血脂水平与脑卒中发病率之间的相关性关系低于血脂水平和冠心病(CHD)的相关性。目的:评估总胆固醇(TC)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C)和甘油三酯水平的地理、种族和民族差异是否与卒中事件的发生相关。方法:从卒中的地理和种族差异的原因研究(REGARDS)中,研究者评估基线无卒中的受试者的LDL-C,HCL-C,TC, non-HDL-C(total- HD
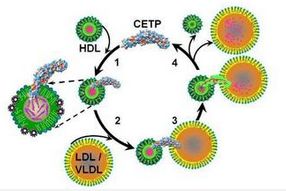
背景:血脂水平与脑卒中发病率之间的相关性关系低于血脂水平和冠心病(CHD)的相关性。
目的:评估总胆固醇(TC)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C)和甘油三酯水平的地理、种族和民族差异是否与卒中事件的发生相关。
方法:从卒中的地理和种族差异的原因研究(REGARDS)中,研究者评估基线无卒中的受试者的LDL-C,HCL-C,TC, non-HDL-C(total- HDL-C)和甘油三酯的水平。应用Cox比例风险模型分析卒中事件和血脂的相关性。对于每个校正血脂(LDL-C、HDL-C、甘油三酯、TC、非HDL-C),研究者计算一系列的增量模型。
结果:分析队列为23867名受试者,平均随访时间事件为7.5±2.9年,1031例发生卒中(874例为缺血性和77例为出血性卒中)。高密度脂蛋白胆固醇基线水平与整体风险降低13%相关(HR 0.87,95% CI:0.81-0.93;出血性卒中为14%和缺血性卒中为16%),和TC与各种卒中风险下降 8%(HR 0.92,95% CI:0.87-0.99)相关。当结果充分校正后,LDL-C、non-HDL-C与缺血性卒中显著相关。当校正年级、种族、年龄*种族、性别、教育、地区或收入后,相关性没有显著差异。
结论:在正常人群中,基线LDL-C和非HDL-C水平与缺血性卒中风险增加显著相关。
原始出处:
Glasser SP, Mosher A, et al. What is the association of lipid levels and incident stroke? Int J Cardiol. 2016 Jun 23
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#非HDL-C#
31
#Cardiol#
28
#缺血性#
39
#缺血性卒#
36
好文值得点赞!继续关注学习。
51
文章很好值得关注
54
#卒中风险#
33
#HDL#
28
#LDL#
30
#HDL-C#
31