Stem Cells Dev:新研究使肝移植成功率大大增加!
2017-10-15 佚名 medicalxpress
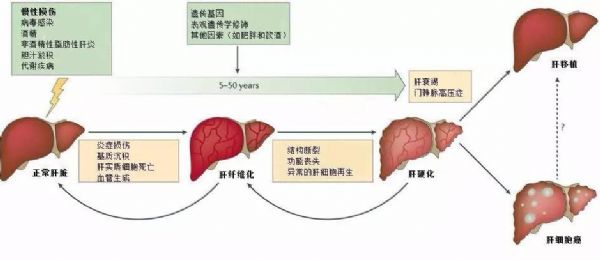
研究人员报道了一种在保留器官的三维结构和细胞外基质(ECM)成分的同时,从整个人肝脏成功地去除细胞物质的方法。他们进一步证明了用人细胞重新喂养这些肝支架的可行性,提供了非破坏性脱细胞方法的概念证明,以生成用于移植的生物工程化肝移植物。该研究发表在干细胞与发育中。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
34
#CEL#
46
#stem cells#
37
#stem cell#
44
#Dev#
31
#STEM#
35
#cells#
42