AAOS|下胫腓联合损伤的生物力学、体格检查、诊断与治疗
2022-02-16 Dr.zhang 骨科青年
踝关节韧带由踝关节侧方韧带和下胫腓韧带两套韧带系统组成,大部分踝关节韧带损伤发生于踝关节侧方韧带,包括三角韧带、距腓前韧带及跟腓韧带等。
踝关节韧带由踝关节侧方韧带和下胫腓韧带两套韧带系统组成,大部分踝关节韧带损伤发生于踝关节侧方韧带,包括三角韧带、距腓前韧带及跟腓韧带等。
下胫腓韧带通常发生于所谓“高能量踝扭伤”,且常合并踝关节骨折。对下胫腓联合损伤,国外学者对其物理检查、诊断与治疗进行了综述,版权归AAOS所有。
一、解剖与生物力学
1.解剖
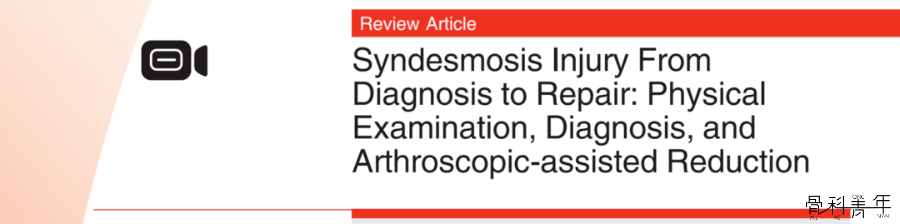
左图:A下胫腓前韧带;B骨间韧带;C距骨;D腓骨;E胫骨;F距腓前韧带;G跟腓韧带。右图:A下胫腓后韧带;B距腓后韧带;C拇长屈肌;D跟骨;E腓骨肌腱。
2.生物力学
下胫腓前韧带起自胫骨远端前外侧的Chaput结节,止于腓骨侧的Wagstaffe结节,是下胫腓稳定结构中最薄弱的部分,在轴向应力下外旋时首先损伤。
下胫腓后韧带起自胫骨远端后外侧的Volkmann结节,止于外踝后方,是下胫腓稳定结构中最强的部分,提供大约35%的下胫腓稳定性。
解剖研究表明,单纯切断下胫腓前韧带后下胫腓分离2.3mm,在此基础上切断骨间韧带后下胫腓分离5.5mm,再切断下胫腓后韧带后下胫腓分离7.3mm。下胫腓联合的作用为维持下胫腓稳定性,对抗旋转、轴向和水平方向的移位。
研究证实距骨向外侧移位1mm即可降低胫距关节接触面积42%,完全的下胫腓损伤可导致关节接触压力增加36%。下胫腓的稳定性对于维持踝关节功能、减少胫距关节退变具有十分重要作用。
二、流行病学
踝关节扭伤占全部运动损伤的10-30%,其中绝大部分为外踝扭伤。
-
随着对下胫腓损伤认识的提高,近期文献报道踝关节扭伤中下胫腓损伤的比例高达17%-74%。
-
下胫腓损伤主要见于高速的碰撞和踝关节背伸位置下外旋应力。
踝关节背伸时距骨的前移迫使下胫腓增宽,在此基础上的外旋应力迫使下胫腓韧带承受异常应力。这一损伤机制在造成严重下胫腓损伤的基础上同样可导致其它韧带损伤。
-
Mait进行了一项尸体研究发现在踝关节背伸、中立和跖屈位置下施加外旋应力,下胫腓韧带损伤的几率分别为100%、50%和0%。三角韧带的深层和浅层在所有下胫腓损伤病例中均有不同程度的损伤。虽然三角韧带对于下胫腓稳定性也有一定的作用,但在Clanton的一项尸体研究中证实除非松解下胫腓前韧带和骨间韧带,否则三角韧带并不影响下胫腓稳定性。
-
17%的外踝扭伤合并不同程度的下胫腓联合损伤。 -
与单纯外踝损伤相比,单纯下胫腓损伤更多发生于对抗性运动。下胫腓联合损伤的恢复时间可超过31天,并导致运动受限和慢性疼痛。
三、诊断
1.病史
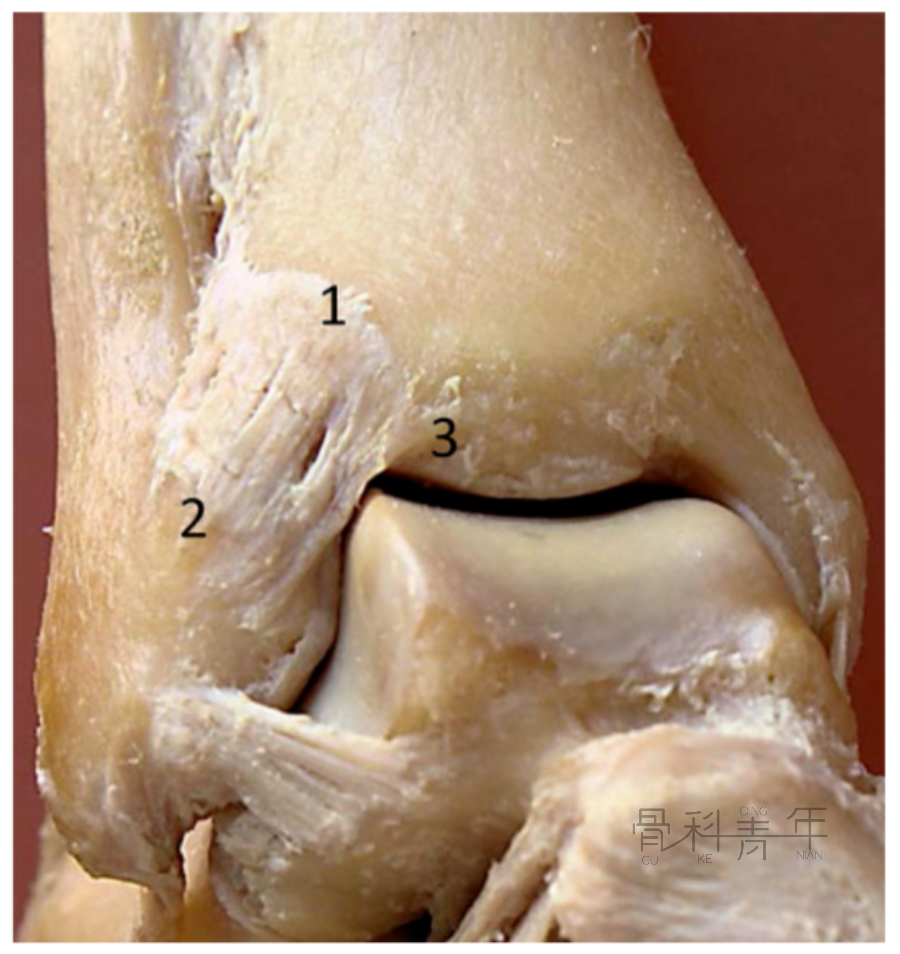
A:交腿试验

B:触诊试验

患者坐位或仰卧位,检查者一手固定胫骨,一手抓住腓骨试图前后移动腓骨。与健侧相比移位超过健侧2~3mm为阳性。

E:外旋应力试验
患者坐位,检查者一手固定胫骨,一手背伸同时外旋踝关节,诱发疼痛为阳性。

F:动态检查

四、影像学评估
-
站立位小腿全长X线可排除踝关节骨折和Maisonneuve损伤,还可进行应力位X线检查,以及负重位X线检查。
-
提示下胫腓损伤的X线征象包括下胫腓间隙增宽,胫腓重叠减少和内踝间隙增宽。
-
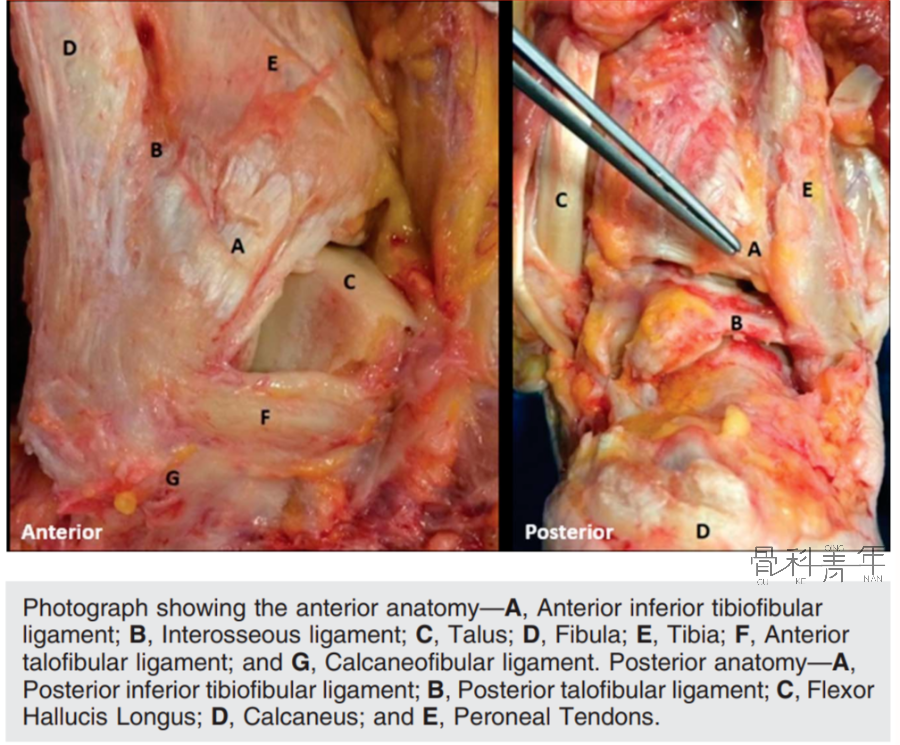
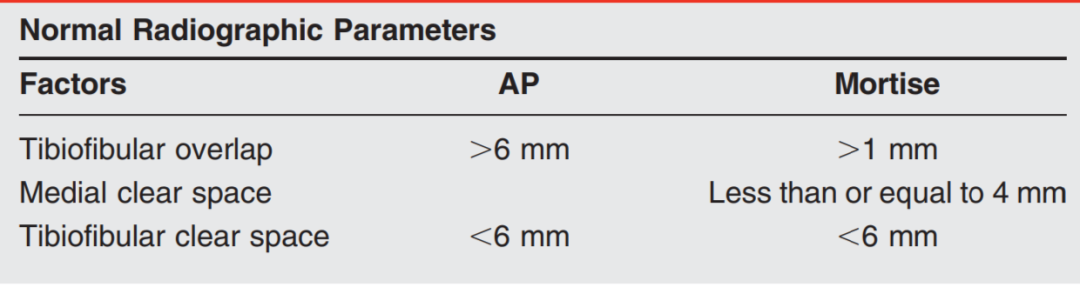
下胫腓间隙的定义为腓骨内侧缘至关节面近端1cm处胫骨腓切迹后缘的距离,如下图,这一间隙在正位和踝穴位X线上距离通常应小于6mm。
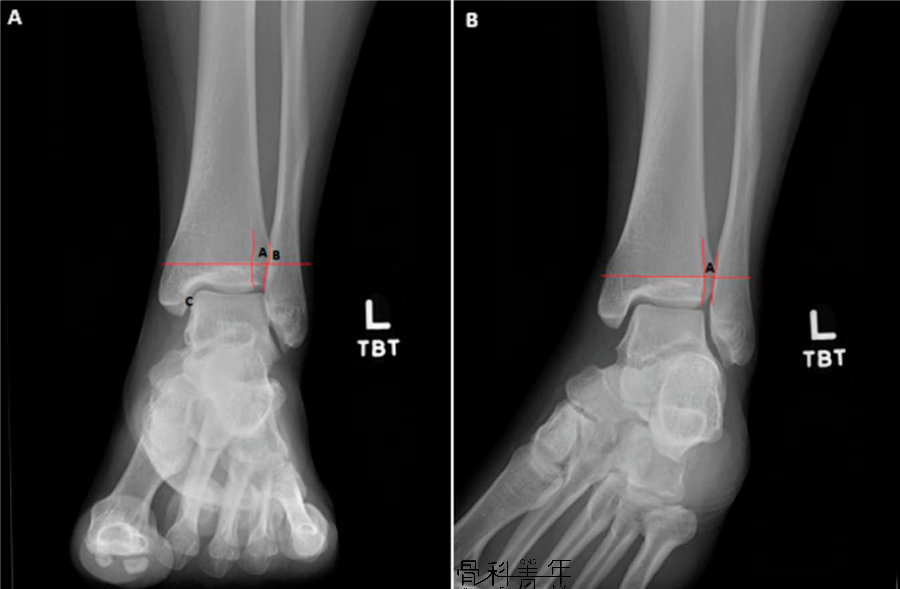
左图:正位X线,其中A为下胫腓间隙,B为下胫腓重叠,C为内踝间隙。右图:踝穴位X线,A为下胫腓间隙。

内踝间隙明显增宽
-
虽然X线是下胫腓损伤最常用的影像学检查,但还是具有明显局限性。
-
MRI检查在下胫腓损伤诊断的敏感性、特异性和准确性分别为100%, 93%和 96%。
-
核磁检查中内踝和下胫腓间隙存在相通的液体信号称为Lambda征,其对于下胫腓损伤的敏感型和特异性分别为75%和85%。
-
MRI检查中发现液体的外溢还可提示骨间韧带损伤(如下图),从而决策手术治疗。

五、麻醉下评估
对于高度怀疑下胫腓损伤而X线和MRI检查为阴性时建议行麻醉下检查。
检查应包括踝关节背伸、背伸外旋应力检查,腓骨平移试验,距骨内外倾斜试验和前抽屉试验。注意检查时上述X线表现。
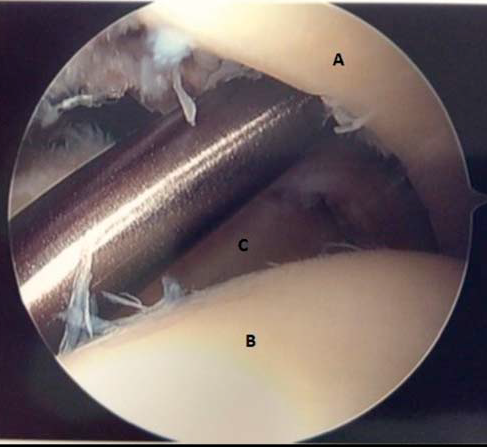
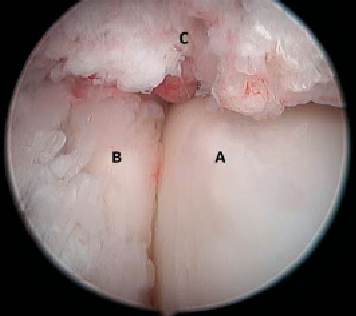
诊断性关节镜检查可明确下胫腓稳定性、软骨缺损情况和三角韧带完整性。关节镜检查还可将直径4.0mm的刮刀放置于下胫腓联合间隙以检查稳定性,如下图。图中A为胫骨,B为距骨,C为腓骨。
六、保守治疗
-
如果没有大体外观的不稳定和影像学的关节分离,可以行保守治疗。
-
外踝扭伤可以早期活动,但下胫腓损伤早期活动会导致下胫腓关节承受不必要的应力。
-
保守治疗首先急性期应制动4天,4-7天保护下逐步限制性负重活动,然后有序进行康复锻炼并恢复体育活动。
-
下胫腓损伤通常要比外踝扭伤恢复时间长。
-
一项橄榄球运动员5年的研究显示恢复时间平均为2.5周,外踝扭伤平均为1.25周。
-
需要指出的是下胫腓损伤的恢复时间可超过31天。
七、手术治疗
下胫腓联合固定的指征是:
-
下胫腓联合损伤伴有不行内固定的腓骨近端骨折或不稳定的内侧损伤;
-
超过踝穴顶5cm的下胫腓联合损伤;
-
下胫腓联合复位后不稳定;
-
陈旧性下胫腓联合分离;
-
对踝关节上方3-5cm的外踝骨折,且内侧损伤(三角韧带)不能修复者,是否固定仍存在争议。
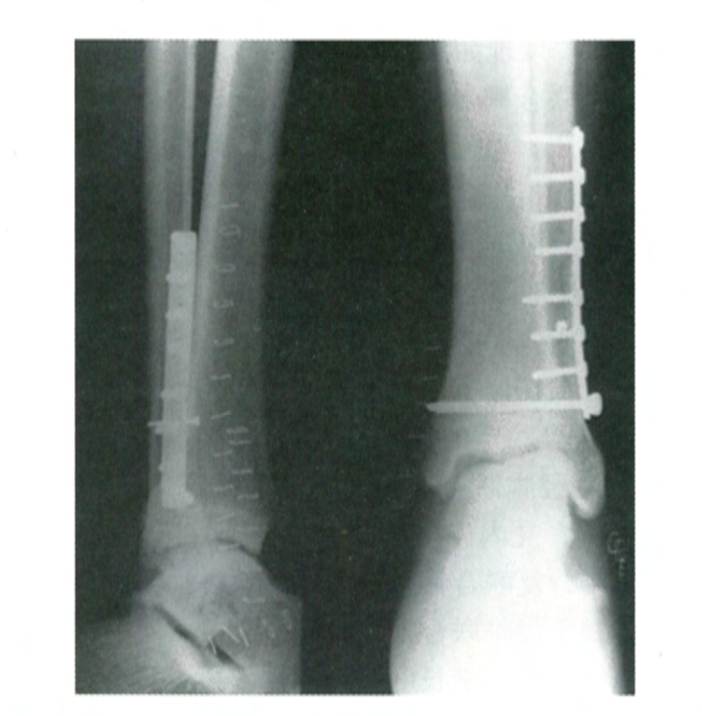
手术治疗下胫腓损伤的第一步为复位下胫腓关节,对不合并腓骨骨折的病例,下胫腓损伤时腓骨通常外旋并外移,复位通常可通过点状复位钳夹腓骨远端后内旋,然后另外一把点状复位钳在胫骨远端关节面近端3cm钳夹腓骨后外侧和胫骨复位,透视证实复位。
当合并Maisonneuve损伤时,应当恢复腓骨的长度、同时内旋并向内侧移位腓骨。合并外踝骨折时,应当首先复位和固定外踝骨折。
-
下胫腓复位后,在踝关节中立位,在胫距关节近端2-5cm处,自外侧平行踝关节关节间隙置入螺钉,同时注意螺钉应从背侧至腹侧约25度-30度夹角固定。 -
螺钉的大小、位置、数量、骨皮质层数对下胫腓损伤手术的影响有很多研究,但没有证据证实较大的螺钉在下胫腓损伤治疗中具有优越性,虽然4.5mm螺钉直径更大,可以提供更大的应力,可以早期取出且断裂可能更小。三层皮质和四层皮质优缺点如下: ① 三层皮质
-
穿三层皮质与穿四层皮质临床效果相似,穿四层皮质螺钉更长,材料更多 -
对皮质骨螺钉,多数螺钉系统以5mm递增,穿四层皮质时可能在螺钉长度选择上过长或过短,并不能精确地穿出第四层皮质; -
四层皮质对下胫腓固定过于牢固,可能影响腓骨正常的外旋活动,使用穿三层皮质螺钉可少固定的强度,为胫腓联合之间的生理活动提供条件。 -
三层皮质的缺点在于,螺钉断钉后难以取出
-
四层皮质能提供更好的稳定性; -
如果发生螺钉断裂,可以从胫骨内侧开窗取出断钉。
-
通常建议韧带愈合后即取出下胫腓螺钉,除非下胫腓螺钉断裂。
-
下胫腓螺钉固定缺点在于具有一定比例的复位不良,这也是患者功能恢复差的重要因素。 -
需要指出的是螺钉本身并不导致复位不良,而仅仅是维持位置。 -
固定之前复位下胫腓关节才是最至关重要的。 -
如果术后的影响提示下胫腓复位不良,取出螺钉有注意下胫腓的复位和恢复下胫腓关节活动度。
2.袢钢板固定
袢钢板固定技术在临床广受欢迎,虽然各种下胫腓固定技术临床效果相仿,袢钢板在生物力学和解剖重建方面具有优势。
-
复位下胫腓后,在关节线近端2cm,由背侧向腹侧倾斜25-30度,类似标准下胫腓螺钉位置置入一枚导针,透视证实导针位置后,空心钻钻透胫腓骨内外侧4层皮质,长方形袢钢板放置于胫骨内侧钻孔处,导针将线缆穿出至腓骨外侧收紧。
-
袢钢板的缺点包括周围骨质溶解和打结固定后缝合结处的疼痛。
-
尸体研究袢钢板降低了下胫腓复位不良的比例,但临床随机对照研究证实袢钢板和下胫腓螺钉两者在下胫腓复位不良方面比例相仿。
-
由于袢钢板存在动态固定机制,2年随访CT证实后袢钢板治疗患者下胫腓复位不良比例明显降低。
-
同时袢钢板还允许下胫腓关节微动,能够重建踝关节背伸时外踝的3度外旋活动。
-
袢钢板的解剖重建还具有避免二次手术取出的优势。
-
研究证实袢钢板固定相比下胫腓螺钉固定具有全负重时间更早、功能评分更高、并发症更少的优势。
-
袢钢板有一项争议在于是否需要两套装置进行固定,研究证实一套袢钢板即可达到下胫腓螺钉固定的效果,附加第二套固定装置并不额外增加稳定性。
一些学者担心袢钢板的微动会导致下胫腓稳定性不足,借鉴外踝韧带缝合修补的经验,有学者建议使用缝合锚修补下胫腓前联合韧带,加强稳定性的同时保留活动度。
-
这一技术最早由Teramoto在2017年报道。
-
Shoji通过尸体研究证实与单纯袢钢板固定并不增加下胫腓稳定性,而下胫腓螺钉固定过于坚强,袢钢板固定加下胫腓前韧带修补可获得与下胫腓解剖完整的尸体标本一样的动态稳定性。
-
这一技术有待于长期临床效果的观察。
-
这一技术在下胫腓切迹浅的患者(25-40%)具有优势,因为较浅的下胫腓切迹先天稳定性不足。

A:下胫腓前韧带重建的胫骨侧Chaput结节;B:腓骨侧Wagstaffe结节
八、并发症
-
手术并发症主要包括下胫腓复位不良和过度加压固定,下胫腓复位不良是下胫腓损伤最重要的并发症,对预后影响最大。 -
复位不良的常见原因为下胫腓切迹形态和点状复位钳放置位置错误。
-
使用点状复位钳时腓骨侧应放置于腓骨嵴,而胫骨侧应放置于侧位透视下胫骨的前1/3。
-
Cherney分析下胫腓切迹认为下胫腓复位不良与下胫腓切迹形态具有明显相关性,切迹较浅的患者容易出现腓骨前移,但很少外旋移位。 -
下胫腓切迹较深是容易出现腓骨后方移位和旋转移位。下胫腓的复位不良可以通过正确方式复位钳得到明显改善,同时可避免过度加压。 -
Haynes定义腓骨向内侧移位与对侧相比超过1mm为过度加压,过度加压的病例平均加压压力为163牛。 -
Lui和Miller描述了通过关节镜证实下胫腓的复位,如下图。图中A为距骨,B为腓骨,C为胫骨。
-
袢钢板固定的一项重要并发症是隐神经和血管损伤,尸体研究证实不管袢钢板放置的如何偏近端,隐神经被勒迫损伤的几率在10-20%,血管在10-37%。操作时进行内侧切口显露胫骨以避免这一损伤。
九、作者推荐方法
-
常规进行临床查体可重力应力下X线及MRI检查,对于高度怀疑下胫腓损伤的患者在术前和术后均进行关节镜检查。
-
对于单纯的下胫腓损伤进行下胫腓前韧带的修补,如果存在三角韧带损伤,同时做三角韧带修补。
-
如果下胫腓前韧带、骨间韧带和下胫腓后韧带都损伤,在透视下复位下胫腓,然后使用袢钢板固定联合下胫腓前韧带修补。
-
如果合并后踝固定,首先使用3.5mm空心钉固定后踝,然后重新进行稳定性评估,根据评估结果按照上述原则进行治疗。
-
术后使用非负重支具进行10-14天固定,2周后穿功能靴部分负重,允许关节活动锻炼。
-
4周时如果走路步态恢复可更换踝关节系带功能靴。
-
6周可以单足跳跃和单足提踵时可逐步恢复跑步和体育运动。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AAO#
44
#AAOS#
45
#诊断与治疗#
45
厉害,非常好,感谢!
44
#损伤#
38
#体格检查#
43
学习了
58