J Orthop Trauma:骨髓干细胞移植对滥用酒精大鼠模型骨折愈合的影响
2013-01-04 J Orthop Trauma 网络 第五十七回
骨折愈合不良是骨外科所面临的极具挑战性的难题之一,据估计骨不连的发生率介于5-20%之间,这对临床工作以及医疗保障系统都带来了极大的困难。以往针对骨不连的临床前期研究模型都主要着眼于导致骨不连的骨质缺损程度。但事实是造成骨不连的原因极其复杂,除了大段骨缺损之外,滥用酒精也是严重影响骨折愈合能力的重要原因之一。有研究发现大约25%-40%的骨折病例在入院时同时并存有酒精中毒的现象,而且研究也发现酒精
骨折愈合不良是骨外科所面临的极具挑战性的难题之一,据估计骨不连的发生率介于5-20%之间,这对临床工作以及医疗保障系统都带来了极大的困难。以往针对骨不连的临床前期研究模型都主要着眼于导致骨不连的骨质缺损程度。但事实是造成骨不连的原因极其复杂,除了大段骨缺损之外,滥用酒精也是严重影响骨折愈合能力的重要原因之一。有研究发现大约25%-40%的骨折病例在入院时同时并存有酒精中毒的现象,而且研究也发现酒精摄取明显与骨折后包括骨不连在内的多种并发症的发生相关。相关研究已经证实,于骨折局部进行干细胞移植有助于大段骨缺损的骨折愈合,而全身性使用干细胞可能也将有利于骨折的愈合。
最近,美国学者Obermeyer TS等采用小鼠胫骨骨折模型探讨了滥用酒精以及体外分离培养的骨髓基质干细胞静脉注射对骨折愈合的影响,相关结果发表于最近一期JOT上。
研究方法如下:
1、6-7周龄的雄性C57BL/6小鼠饲养至9周龄后进行酒精滥用造模,其具体方法为:以酒精/生理盐水体积容量为20%的酒精按2g/kg的标准经胃肠道饲喂小鼠,连续3天后停止4天,然后再次连续使用3天,再停止4天,共2周时间以制造滥用酒精(BAC)模型。而对照组则以纯生理盐水按相同的方法进行处理;
2、从7-8周龄的表达绿色荧光蛋白(GFP)的转基因C57BL/6小鼠(C57BL/6-Tg-UBC-GFP-30Scha/J)的胫骨和股骨采集骨髓组织,经相应处理后分离出骨髓基质干细胞并进行培养,经验证所获得的细胞(MSC-GFP)具有三系分化能力后通过小鼠尾静脉注入胫骨骨折造模成功后24小时的小鼠体内;
3、注射24小时(骨折48小时)后开始进行在体荧光扫描检查,每日1次,共14天,每一组动物检查5-6只;、
4、14天后收集伤肢标本进行体外研究,骨痂标本经适当处理后进行以下检查:免疫组化、组织学、微CT扫描、以及生物力学测定。
研究结果如下:
1、伤后2天,注射MSC-GFP的对照组动物胫骨骨折部荧光检查阳性,伤后2-3天时达高峰,而无骨折的胫骨则为阴性;而注射MSC-GFP的实验组动物则于伤后3天发现骨折部荧光阳性,骨折后3-4天达峰值;随后两组动物的荧光强度均随时间延长而减弱,约于骨折后7天降至伤前水平;
2、免疫组化检测发现注射MSC-GFP的小鼠骨痂内有抗GFP的亲和素生物素过氧化物酶复合物反应;微CT扫描发现滥用酒精小鼠的骨痂量较对照小鼠少69%,;滥用酒精小鼠中注射MSC者的骨痂量较未注射者多165%,而与对照组的骨痂量相似,但不同组别小鼠骨痂的骨密度无明显差别;
3、生物力学检测结果如下:滥用酒精小鼠的抗弯曲强度明显低于对照组,并且滥用酒精也降低了骨痂的刚度;滥用酒精小鼠中,注射MSC者胫骨的抗弯曲强度较未注射者明显增高,但两者骨痂的刚度并无明显差别;
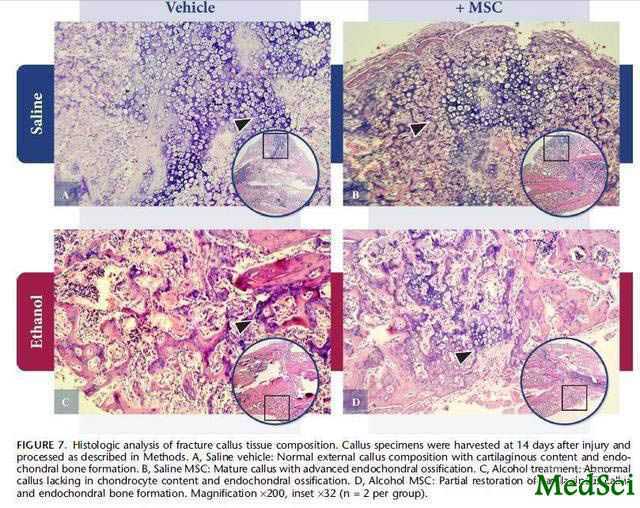
4、组织学检测结果如下:对照组小鼠标本存在正常的软骨内化成骨性的外骨痂,注射MSC后则发现了更多外观更加成熟的提示软骨内化成骨性的外骨痂;与此相反的是,滥用酒精小鼠的标本中缺乏软骨性外骨痂以及软骨内化骨的形成,而仅仅存在由外骨膜来源的骨痂组织,但滥用酒精的小鼠接受MSC移植后则部分地恢复了软骨性外骨痂的形成。
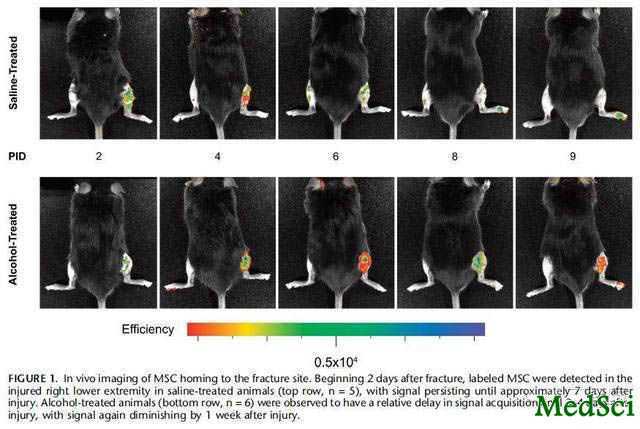
图1 骨折部标记MSC的定植情况的在体研究结果。骨折后2天,对照组小鼠伤肢(右下肢)即可探测到标记的MSC,并且直到伤后约7天时均能探测到(上排,n=5)。而酒精滥用模型小鼠(下排,n=6)则显示标记MSC的出现于相对较晚的伤后3-4天,但同样于伤后1周左右消失
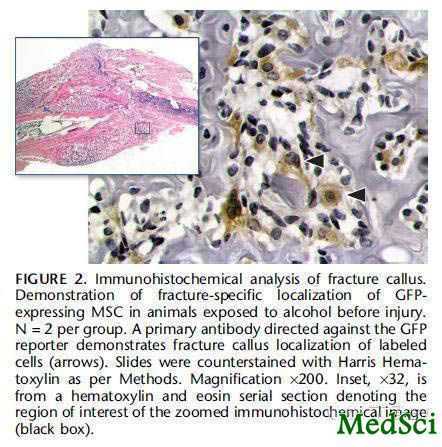
图2 骨痂的免疫组化检测结果。图示实验组动物接受MSC移植组骨痂内GFP标记MSC的定植情况。
箭头所示为GFP特异性一抗与其结合后的检测结果
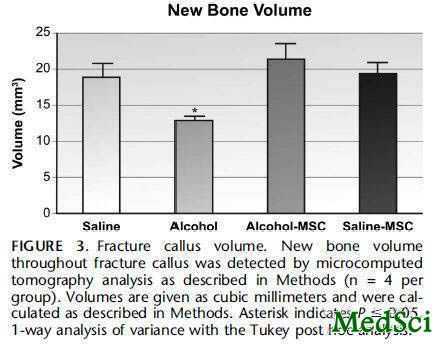
图3 各组动物骨折部骨痂体积的测定结果
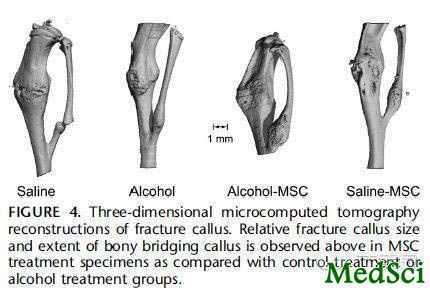
图4 伤肢微CT扫描三维成像结果,显示实验组和对照组动物接受或不接受MSC移植后的骨痂形成情况

图5 骨痂组织的生物力学测定结果
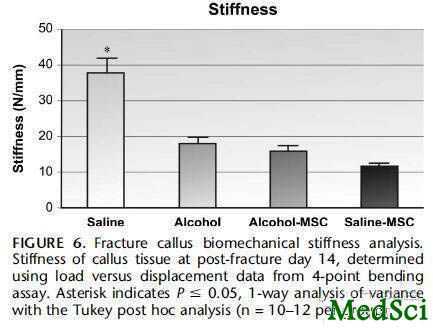
图6 骨痂组织刚度的测定结果
通过上述研究,Obermeyer TS等认为,酒精滥用会明显降低骨折的修复,表现为减少骨痂的形成以及软骨内化骨的产生,并降低骨痂强度,但这些现象能大部分被全身应用MSC所逆转,提示这些细胞能够定植于骨折部位从而有利于骨折的修复。这可能为将来临床上更加有效地治疗骨折愈合障碍提供新的方式。
Mesenchymal Stem Cells Facilitate Fracture Repair in an Alcohol-Induced Impaired Healing Model
Objectives
Clinical studies have shown alcohol to be a risk factor for traumatic orthopaedic injuries and for nonunion. Data from animal studies suggest that alcohol exposure inhibits fracture healing. This report presents a novel rodent model of impaired fracture healing caused by repeated alcohol exposure. Using this model, we examined the regenerative effects of an intravenously administered population of isolated and expanded mesenchymal stem cells (MSCs) on fracture healing.
Methods
Bone marrow–derived MSC were isolated from transgenic green fluorescent protein C57BL/6 mice, and culture expanded using a lineage depletion protocol. Adult wild-type C57BL/6 mice were subjected to a 2-week binge alcohol exposure paradigm (3 days during which they received daily intraperitoneal injections of a 20% alcohol/saline solution followed by a 4-day rest period and another binge cycle for 3 consecutive days). At completion of the second binge cycle, mice were subjected to a mid-shaft tibia fracture while intoxicated. Twenty-four hours after the fracture, animals were administered an intravenous transplant of green fluorescent protein–labeled MSC. Two weeks after the fracture, animals were euthanized and injured tibiae were collected and subjected to biomechanical, histologic, and microcomputed tomography analysis.
Results
Pre-injury binge alcohol exposure resulted in a significant impairment in biomechanical strength and decrease in callus volume. MSC transplants restored both fracture callus volume (P < 0.05) and biomechanical strength (P < 0.05) in animals with alcohol-impaired healing. In vivo imaging demonstrated a time-dependent MSC migration to the fracture site.
Conclusions
These data suggest that a 2-week binge alcohol exposure significantly impairs fracture healing in a murine tibia fracture model. Intravenously administered MSC were capable of specifically homing to the fracture site and of normalizing biomechanical, histologic, and microcomputed tomography parameters of healing in animals exposed to alcohol. Understanding MSC recruitment patterns and functional contributions to fracture repair may lead to their use in patients with impaired fracture healing and nonunion.
{nextpage}本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
38
#Trauma#
31
#骨折愈合#
47
#细胞移植#
32
#滥用#
28