大网膜扭转CT病例图片影像诊断分析
2019-02-15 佚名 放射学实践 影像园
患者,男,50岁,因腹痛2天入院。查体:右腹部压痛、反跳痛,以右下腹为甚,无肌紧张,无恶心、呕吐,无畏寒、发热,无尿频、尿急、尿痛等不适;其余查体未见特殊。既往史:15年前因阑尾炎行保守治疗。血常规白细胞计数10.46*109g/l。
【临床病史】:
患者,男,50岁,因腹痛2天入院。查体:右腹部压痛、反跳痛,以右下腹为甚,无肌紧张,无恶心、呕吐,无畏寒、发热,无尿频、尿急、尿痛等不适;其余查体未见特殊。既往史:15年前因阑尾炎行保守治疗。血常规白细胞计数10.46*109g/l。
【影像图片】
CT图像

【影像诊断】:
大网膜扭转(torsion of greater omentum)
【临床治疗】:
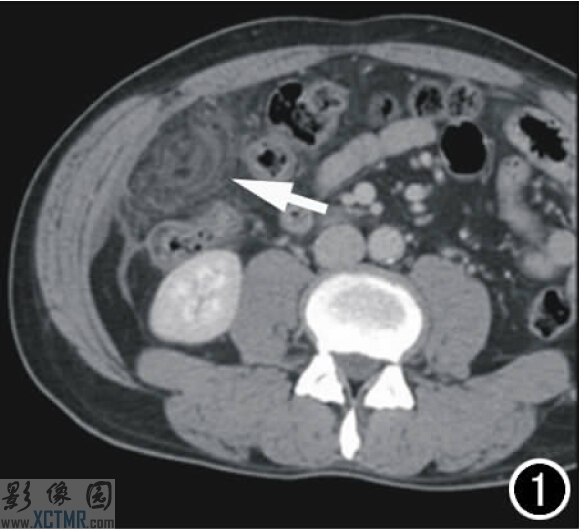
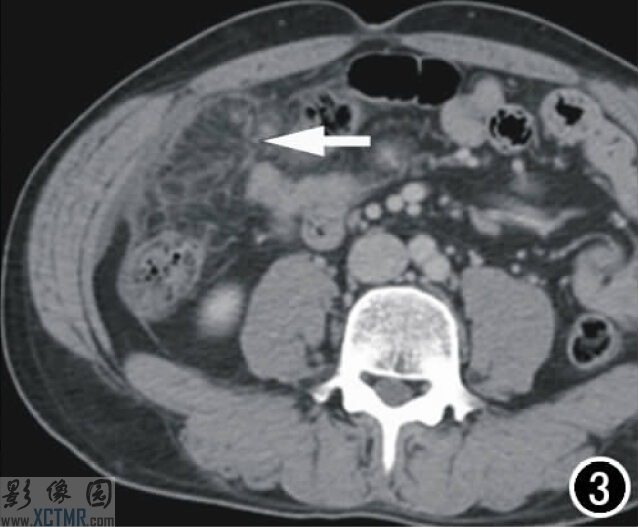
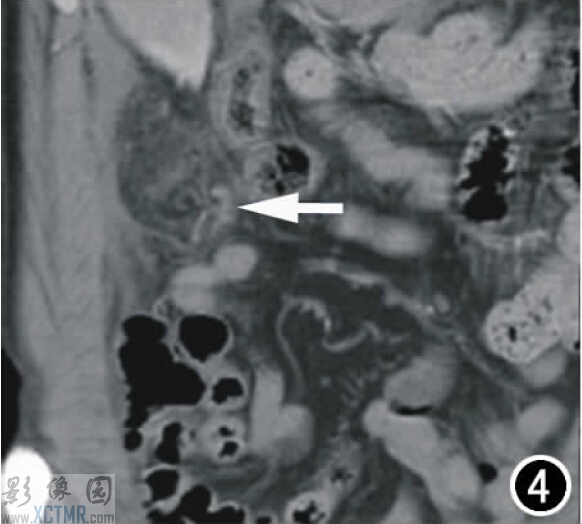
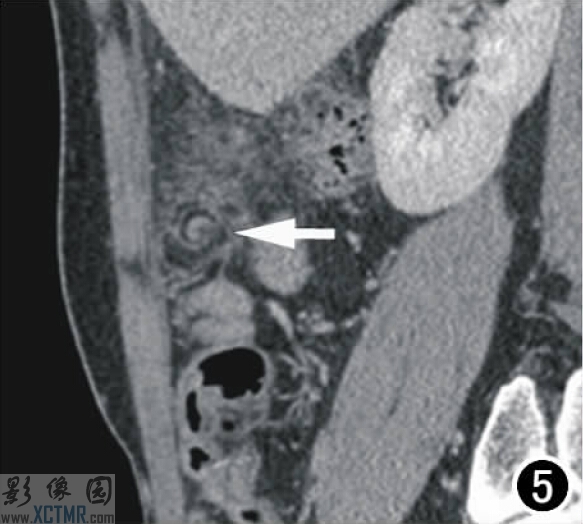
经抗炎治疗2天,患者腹痛无明显缓解,有加重趋势,且腹痛范围扩大,累及整个右侧腹部,呈持续性钝痛,难以忍受。查体:体温正常,右侧腹压痛、反跳痛明显,有肌紧张,腹膜炎体征重。再次急诊腹部增强CT示右中上腹腔脂肪间隙大网膜区域团状、条索影(图1-5),较之前增加,考虑脓肿形成。遂行急诊剖腹探查。术中见右侧中上腹腔大网膜、肠系膜、部分回肠与右侧腹壁致密粘连;松解粘连后见约15cm*12cm区域大网膜发黑坏死,坏死部分大网膜的血管扭转2圈(图6),右侧中上腹腔结肠旁沟有约20ml略浑浊腹水。手术行大网膜扭转复位,并切除坏死部分大网膜。术后病理为大网膜及坏死组织。图6 术中见大网膜局部呈螺旋状扭转(箭),部分缺血发黑。
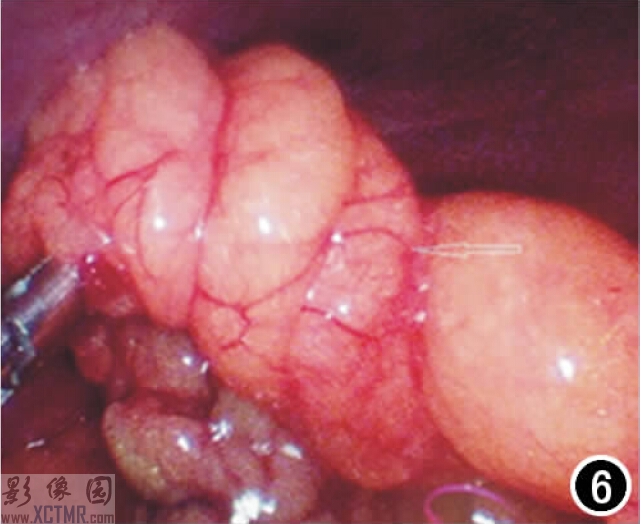
大网膜扭转6
【术后诊断】:
原发性大网膜部分扭转并坏死,局限性腹膜炎。
【讨论】:
大网膜扭转是少见的急腹症,主要临床症状为突发性腹部,多呈绞痛,持续进行性加重,可并发胃肠道症状,如恶心及呕吐,活动可使疼痛加重。腹部检查有压痛、反跳痛、肌紧张。体温多不升高或轻微升高,白细胞正常或稍增高,但缺乏特异性,常误诊为急性阑尾炎、胆囊炎、腹膜炎、胃肠穿孔等。
本病于1899年首次报道,至今共报道300余例,仅1例术前以CT检查作出正确诊断,术前误诊率接近100%。本病常见于中青年,以20-50岁中青年居多,儿童及老年人极少见,男性较女性多见,男女比例为2:1。根据发生的原因分为原发性和继发性。原发性大网膜扭转一般认为与大网膜的解剖形态异常(如过长)、位置改变(如剧烈运动、突然改变体位、过饱后引起的胃肠蠕动、腹内压力的改变)有关;继发性即继发于其它疾病,如腹腔肿瘤、炎症等。常规检查手段如X线平片、超声对其诊断意义不大,MRI诊断国内未见相关报道。CT诊断报道少见,通常CT检查能够排除有无其它上述急腹症和原发疾病,但对大网膜扭转本身的征象认识不足,容易误诊。
结合本病例CT表现及以往文献,大网膜扭转的CT征象有以下特点:① “星云征”或“星团征”,即扭转的大网膜呈团状,但内部较分散,是由于其内的较多网膜结构、血管及脂肪发生水肿、渗出所致,其内结构较紊乱、密度不均匀。② “假包膜征”,其边缘可见假包膜包绕,可能为相邻脏层腹膜或网膜包裹形成,扭转点假包膜常不完整、不规则。③“漩窝征”,通常在扭转的大网膜根部可见增粗旋转的系膜血管呈漩窝状。本病例在大网膜扭转根部的短轴切面(非人体轴位)较好显示。④“集束征”或“花瓣征”,在扭转的大网膜根部的长轴切面上可见增粗的网膜结构向扭转点聚集,呈束状。为了便于显示上述影像细节,要对CT图像进行多平面重组(MPR),并对局部进行1mm薄层重组。
大网膜扭转常导致系膜血管被压迫,容易发生缺血坏死,早期准确诊断意义重大。大网膜扭转的CT表现具有一定特征性,随着病例的积累,CT有望成为诊断大网膜扭转的有效手段。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习了,谢谢
50
#CT病例#
50
学习了
55
#影像诊断#
41
受教了!
57