结节性硬化性综合症之多灶性微小结节样肺细胞增生(MMPH)一例
2022-09-17 放射沙龙 放射沙龙
TSC 存在进行性多器官受累的特性,早期诊断意义重大,以脑外受累器官病变首诊误诊率高。
【病史】
女,36岁,偶然体检发现肺部异常病变。


上面两幅HRCT示两肺多发的随机分布大小不等磨玻璃结节灶。
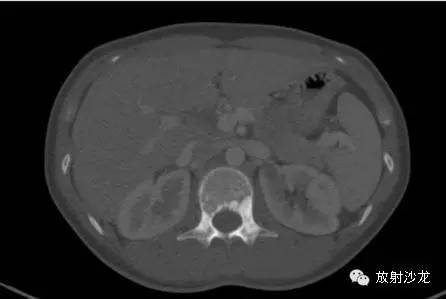
腹部CT示腰椎骨质内可见象牙样骨质硬化,左肾内可见边界清晰的低密度结节灶。

增强扫描示左肾病灶内含脂肪密度,周围可见花边样强化,其内可见分隔。
(胸腔镜活检和病理诊断结果肺部病变为多灶性微小结节样肺细胞增生( MMPH)、左肾病变为肾血管平滑肌脂肪瘤。)
【讨论】
1、结节性硬化综合症(TSC)又称 Bourneville-Pringle病,全身多器官组织缺陷和良性结缔组织错构瘤是 TSC的组织病理基础,除外周神经骨骼肌、松果体外可累及所有的组织器官, 以皮肤神经系统受累为主, 有家族性发病倾向和年龄遗传效应。
2、TSH临床特点:
TSC 多见于儿童,典型临床表现为 Vogt 三联征(癫痫、智力低下、皮脂腺瘤)。
TSC 累及肾脏与肝脏多为偶然发现,以此首诊临床容易误诊或漏诊,其症状出现与病变瘤体大小及并发症相关,可增加肾脏自发性出血和肾癌的危险性,肾脏病变被认为是 TSC 最常见的死亡原因。
3、影像特点和病理基础:
脑内改变: 神经系统硬化结节病理上由胶质细胞异常的成神经细胞、成胶质细胞、神经节细胞等组成, 常有钙化。影像表现具特征性:( 1) 室管膜下多发结节,为多发对称性分布,钙化结节具特征性;( 2) 皮质或皮质下结节,以额顶叶多见;( 3) 脑白质区异常信号,呈放射状、楔形或不定形稍长 T2 信号影为特征,T2WI-FLAIR 上显示明显结节呈等或稍高密度及等 T1稍长 T2信号,增强扫描不强化或强化不明显,当结节增大且出现明显强化时应考虑恶变为室管膜下巨细胞星形细胞瘤,后者多位于透明隔和孟氏孔区,CT 是发现室管膜下钙化结节最敏感的检查方法,文献报道,对于临床高度怀疑 TSC 的患者,CT 可以作为 TSC 初筛诊断的首选方法。
脑外改变:
( 1) TSC 合并肝、肾AML: TSC 肝、肾AML 以瘤内含脂肪成分为特征,增强扫描瘤体实性部分明显强化且强化持续时间较长, 瘤体随时间推移而增大、80% TSC 合并双肾多发的AML,TSC中肝 AML 与双肾AML具有显著的相关性,二者结合提示 TSC。
( 2) TSC 肺部病变:包括 MMPH和LAM,MMPH组织学上为增生的II型肺泡细胞, 表现为弥漫分布小结节状密度增高影伴小叶间隔增厚; LAM 主要表现为血管平滑肌的异常增殖,表现为薄壁( < 3mm) 清晰的肺囊肿且均匀分布于全肺。
( 3) TSC 骨骼改变:病理机制可能与骨骼生长骨化过程中成熟骨小梁发生融合而不能再吸收、塑型,结果导致致密骨斑样发育异常有关。特征性骨骼影像表现为椎体内多发硬化小结节伴象牙质样椎弓硬化;研究同时发现,骨质改变以腰椎多见且最先累及,且首先累及附件,椎体病变多位于其后半部, 骨质硬化并体积增大见于晚期病例。颅骨病变以板障改变为主,近内板侧明显,部分伴局部体积增大。结果显示,本病骨质改变具有多骨多发且进行性加重特点。本病需与肾性骨病、成骨转移性骨肿瘤、烛油样骨质增生症鉴别。
TSC 存在进行性多器官受累的特性,早期诊断意义重大,以脑外受累器官病变首诊误诊率高,临床医师应提高认识,熟悉 TSC 临床及相关受累器官的影像特征,及早发现和处理或干预受累器官潜在的威胁生命的合并症。CT 与MRI在 TSC 的诊断及随访中具有十分重要的价值, 具有风向标作用,脑内改变具特征性且MRI价值突出, 脑外改变值得重视且具有一定的影像特征及明显的临床价值。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#结节性#
44
#小结节#
39
#肺细胞#
37
#多灶性#
42
#硬化性#
44