J Clin Periodontol:慢性牙周炎发病率和严重程度评估应该标准化
2015-04-03 MedSci MedSci原创
J Clin Periodontol:慢性牙周炎发病率和严重程度评估的标准化关键词:慢性牙周炎 刘性病学研究 患病率 标准原则 监测近日EU/USA牙周流行病学工作组联合对牙周炎的患病率和严重程度的评估制订了标准,相关文章于2015年3月23日在线发表于JOURNAL OF CLINICAL PERIODONTOLOGY《临床牙周病杂志》。牙周病普遍存在于各国,但是各国人群的患病率及严重程度各异。

近日EU/USA牙周流行病学工作组联合对牙周炎的患病率和严重程度的评估制订了标准,相关文章于2015年3月23日在线发表于JOURNAL OF CLINICAL PERIODONTOLOGY《临床牙周病杂志》。
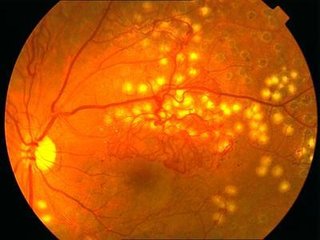
牙周病普遍存在于各国,但是各国人群的患病率及严重程度各异。然而,患病率及严重程度的评估却受测定方法的影响,包括测定技术,患者的评定,牙周检查协议以及不同的口腔健康状况。结果,严重阻碍了各国人群之间的牙周炎严重程度的对比,也很难对全球牙周炎患病率的变化得出推论。
为了克服这个局限性,研究人员建议应当在未来流行病学调查中对牙周炎的患病率和严重程度的评估制定标准原则。这些原则包括研究设计的综合报告,记录协议,个体相关和口腔的特异性数据。此外,应当在总人群中以及特定的年龄组中排列牙周数据。牙周数据包括临床附着丧失(CAL)的程度以及患病率,探诊深度(PD),平均CAL/PD,CDC/AAP病例定义,探诊出血指数。在未来的研究中,这些措施的实施将会提高报导质量,使得不同国家人群中牙周炎的患病率和严重程度具有对比性,并能为导致牙周炎患病率和严重程度的决定因素提供更好的观察视角。
为了帮助研究人员、流行病学家以及其他健康数据使用者更好的处理获得的数据信息,我们建议一些关键的项目以及重要性的排名应该在出版物的主要章节或者在线列出。
原始出处:
Holtfreter B, Albandar JM, Dietrich T, Dye BA, Eaton KA, Eke PI, Papapanou PN, Kocher T. Standards for reporting chronic periodontitis prevalence and severity in epidemiologic studies Proposedstandards from the Joint EU/USA Periodontal Epidemiology Working Group.J Clin Periodontol.2015 Mar 23. doi: 10.1111/jcpe.12392.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











好文章,还会关注
68
#标准化#
23
#PE#
36
#发病率#
23
有道理
176
#慢性牙周炎#
46
#牙周#
30
有道理,
135
值得了解
126