Neurology:血清神经丝光与那他珠单抗治疗的复发缓解型多发性硬化患者病情进展的关系
2021-09-24 Naomii MedSci原创
研究人员就血清神经丝光蛋白 (NFL)对复发性缓解型多发性硬化症(RRMS)患者应用那他珠单抗治疗后反映或预测病情进展的可能性进行了讨论,未能捕捉或预测病变进展,病变进展独立于炎性/影像改变。
多发性硬化(MS)是一种慢性炎性的中枢神经系统退行性疾病。在10-15年的疾病演变过程中,大多数患者发生的进行性不可逆的残疾极大地独立于急性局灶性炎性活动,包括复发和MRI新发损害。随着治疗复发-缓解型多发性硬化症(RRMS)的高效疾病修饰疗法(DMT)的出现,大多数患者的急性局灶性炎症性疾病活动可以被缓解。当前证据表明,继发性进展性多发性硬化症(SPMS)患者的残疾增加可以发生在疾病发作时,而与急性局灶性炎性活动无关。这些过程的分离表明,潜在的进展机制至少部分地独立于那些引起复发相关的神经轴突损伤的机制。
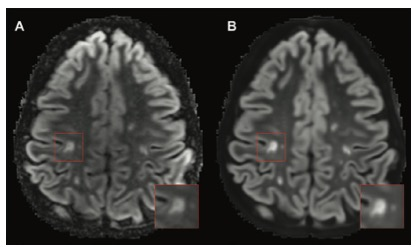
神经丝光(NFL)是神经轴突损伤的生物标志物,在RRMS患者复发期间升高,并伴随着新的T2/GE MRI病变的出现,在急性事件发生后几个月内恢复到基线,并在接受DMT后开始下降。在已有的横断面研究中,NFL与疾病严重程度的衡量标准,如扩展的残疾严重程度评分(EDS)相关。由此,NFL是一种监测MS急性局灶性炎症性疾病活动并预测短期、长期神经功能障碍的潜在有力指标。近日,有研究人员就血清神经丝光蛋白 (NFL)对复发性缓解型多发性硬化症(RRMS)患者应用那他珠单抗治疗后反映或预测病情进展的可能性进行了讨论。
该研究是一项前瞻性的队列研究,纳入的RRMS患者均满足≥18岁且接受那他珠单抗治疗并接受至少3年随访。每年进行一次临床和MRI评估,并在随访期间的5个时间点(包括启动那他珠单抗治疗当天、3个月、1年和2年以及最后一次随访)测定血清神经营养因子(NFL)水平。在一般线性回归模型下,研究者比较了第1年就诊和末次随访时,有/无EDSS进展的患者的NFL纵向改变,并对有无EDSS+进展的患者进行对比,EDSS进展是一个综合终点,包括EDSS、9孔手功能测试和定时25英尺步行。
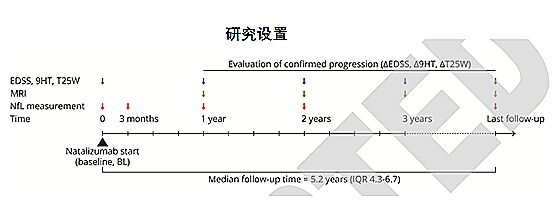
研究共纳入89例受试者。纳他珠单抗治疗后的中位随访时间为5.2年(IQR 4.3~6.7,范围3.0~11.0),平均年龄为36.9岁(SD:8.5),中位病程为7.4年(IQR 3.8~12.1)。
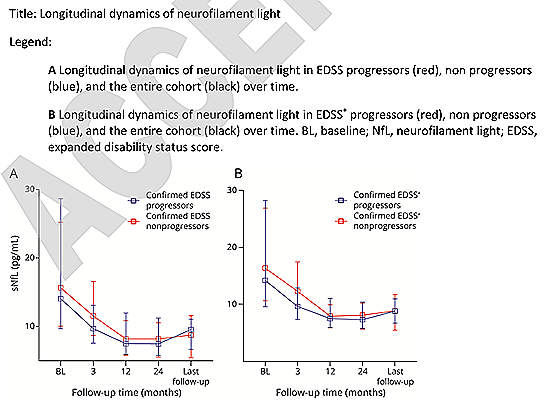
- 从第1年到末次随访,28/89(31.5%)的患者出现了确认的EDSS进展。89名患者中有73名获得了EDSS+终点的数据,其中35/73(47.9%)显示出确认的EDSS+进展。
- 在接受那他珠单抗治疗3个月后,NFL水平显著下降,开始治疗1年后降至基线水平的50%即最低点。l 进行者和非进行者的NFL纵向动力学没有差异。基线和纳他珠单抗治疗后一年的NFL水平并不能预测最后一次随访的进展。
在该研究队列中,NFL未能捕捉或预测病变进展,病变的进展极大地独立于急性局灶性炎性活动的临床或影像学改变。因此,可能需要额外的生物标志物来监测这些患者的进展。
文献来源:https://n.neurology.org/content/early/2021/09/09/WNL.0000000000012752.long
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#病情#
47
#神经丝#
36
#Neurol#
40
#那他珠单抗#
40
#多发性#
31