ESC2015:NSTE-ACS指南诊断和监测要点
2015-09-07 大鹏 译 医学论坛网
2015欧洲心脏病学会年会(ESC2015)专题报道一、诊断及风险分层要点1.新指南推荐,医生应综合患者病史、症状、体征、体格检查其他要点、心电图检查(ECG)及实验室检查结果等多方面信息,作出诊断并评估患者短期缺血及出血分层情况。(推荐等级Ⅰ,证据等级A)2.推荐患者首次医疗接触后10分钟之内接受12导联ECG检查,并邀请有经验的临床医生解读ECG检查结果。另外,若患者再发症状或存在诊断不确定性
一、诊断及风险分层要点
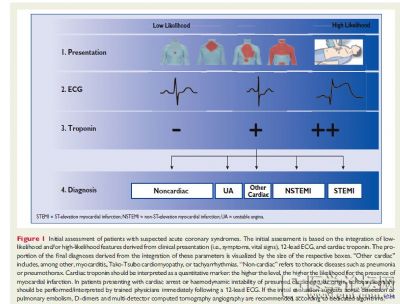
1.新指南推荐,医生应综合患者病史、症状、体征、体格检查其他要点、心电图检查(ECG)及实验室检查结果等多方面信息,作出诊断并评估患者短期缺血及出血分层情况。(推荐等级Ⅰ,证据等级A)
2.推荐患者首次医疗接触后10分钟之内接受12导联ECG检查,并邀请有经验的临床医生解读ECG检查结果。另外,若患者再发症状或存在诊断不确定性,推荐复查12导联ECG。(推荐等级Ⅰ,证据等级B)
3.若怀疑患者存在持续缺血,且标准导联ECG结果无法确诊,推荐复查相应导联ECG检查,包括V3R,V4R,V7,V8及V9。(推荐等级Ⅰ,证据等级C)
5.若患者能接受高敏心肌肌钙蛋白检查,推荐在0小时及3小时两个时间点行快速排除法诊断(rule-out protocol)。(推荐等级Ⅰ,证据等级B)
6.若患者能接受高敏心肌肌钙蛋白检查,且存在有效的0h/1h算法(0 h/1 h algorithm),推荐在0小时及1小时两个时间点行快速排除法诊断及确诊诊断;若前两次检查无法确诊,而患者又高度疑似急性冠脉综合征(ACS),推荐在3至6小时之间复查。(推荐等级Ⅰ,证据等级B)
7.推荐使用已有的评分工具评估患者预后。(推荐等级Ⅰ,证据等级B)
8.对于正接受冠脉造影术的患者,可考虑使用CRUSADE评分定量评估出血风险。(推荐等级Ⅱb,证据等级B)
二、影像学检查要点
1.对于无复发性胸痛的患者,若患者ECG及心肌肌钙蛋白均正常,但疑似ACS,在制定有创性诊疗策略前,推荐进行配有影像的微创应激试验以确定可诱导的缺血情况。(推荐等级Ⅰ,证据等级A)
2.推荐行超声心动图检查评估患者局部及全左心室功能情况,以资鉴别诊断。(推荐等级Ⅰ,证据等级C)
3.若患者存在低中度冠心病可能性,且ECG及心肌肌钙蛋白检查无法确诊,可考虑多排螺旋CT(MDCT)冠脉造影是一种可选的有创性影像学检查,用以ACS排除诊断。(推荐等级Ⅱa,证据等级A)
三、监测要点
1.在患者非ST段抬高型心肌梗死(NSTEMI)诊断结果明确前,推荐行连续心律监测。(推荐等级Ⅰ,证据等级C)
2.推荐将NSTEMI患者移至监测中心治疗。(推荐等级Ⅰ,证据等级C)
3.对于心律失常低危的NSTEMI患者,可考虑心律监测(最长24小时)或PCI治疗。(推荐等级Ⅱa,证据等级C)
4.对于心律失常中高危的NSTEMI患者,可考虑超过24小时的心律监测。(推荐等级Ⅱa,证据等级C)
5.若患者无持续性缺血体征或症状,对于特定患者群体(如疑似冠脉痉挛,存在心律失常相关事件),可考虑在不稳定心绞痛时行心律监测。(推荐等级Ⅱb,证据等级C)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#NSTE-ACS#
34
#NSTE-ACS指南#
26
#NST#
33
#ACS#
27