2016黑色素瘤治疗进展汇总
2016-08-09 MedSci MedSci原创
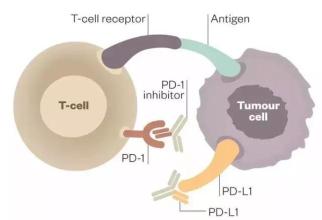
黑色素瘤,又称恶性黑色素瘤,是来源于黑色素细胞的一类恶性肿瘤,常见于皮肤,亦见于黏膜、眼脉络膜等部位。在亚洲人和有色人种中,原发于皮肤的黑色素瘤占50%~70%,最常见的原发部位为肢端(约占所有黑色素瘤的50%),即足底、足趾、手指末端及甲下等部位,其次为粘膜黑色素瘤(约占20%左右),而欧美白种人这两种亚型仅占所有黑色素瘤的5%。黑色素瘤是皮肤肿瘤中恶性程度最高的瘤种,容易出现远处转移。早期
本文系梅斯医学(MedSci)原创编译整理,欢迎转载!更多资讯,请下载"辣眼睛的医学科研神器之梅斯医学APP”!扫一下二维码即可:

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#色素#
41
总结的很全面!
46
分享一下!!
0
早期诊断和治疗因而显得尤为重要!!!!
58
了解了!!
54
继续关注
61
继续学习
30
#黑色素#
24
#黑色素#
28
我会继续一直关注!希望科研工作者们继续努力,早日攻克癌症!早日解救百姓于水火!
24