JCEM:肽受体放射性核素治疗(PRRT)治疗转移性副神经节瘤/嗜铬细胞瘤的疗效
2017-06-17 MedSci MedSci原创
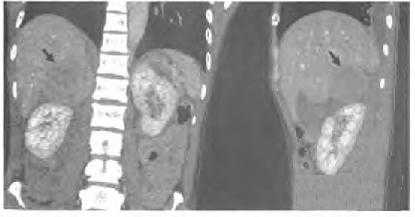
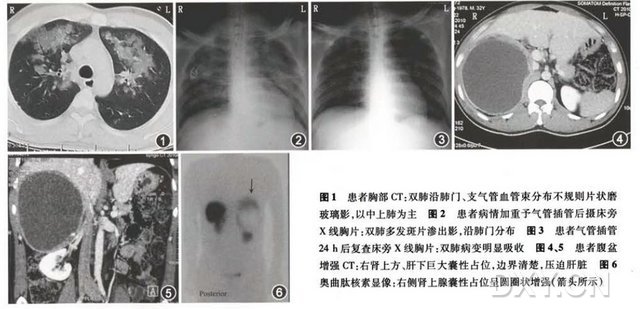
肽受体放射性核素治疗(PRRT)是一种与分子有关的治疗(也叫做放射性同位素治疗)被用来治疗特定的癌症类型,叫做神经内分泌恶性肿瘤或者神经内分泌性肿瘤(神经内分泌肿瘤)。肽受体放射性核素治疗(PRRT)也是正在被研究作为前列腺和胰腺肿瘤治疗方法。对于不能手术切除的副神经节瘤(PGL)/嗜铬细胞瘤(PCC)患者的治疗选择是有限的,尤其是在出现难控制的继发性高血压(HTN)患者中。既往的研究表明,使用P
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#核素治疗#
34
#JCE#
29
#JCEM#
18
学习了谢谢分享!!
65
vv不哼哼唧唧就好好
60
#转移性#
19
#细胞瘤#
18
#副神经节瘤#
22
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦
63
学习了,谢谢分享
51