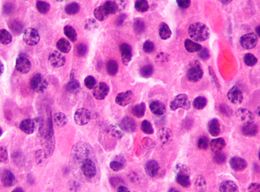
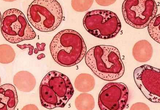
复发性/难治性多发性骨髓瘤患者的福音:Elotuzumab疗法
2015-08-20 MedSci 译 MedSci原创
Elotuzumab是一种靶向淋巴细胞活化分子F7信号的免疫刺激单克隆抗体。它联合来那度胺和地塞米松治疗复发性/难治性多发性骨髓瘤患者在一项1b-2 期的研究中显示了良好的疗效。
背景:Elotuzumab是一种靶向淋巴细胞活化分子F7信号的免疫刺激单克隆抗体。它联合来那度胺和地塞米松治疗复发性/难治性多发性骨髓瘤患者在一项1b-2 期的研究中显示了良好的疗效。
研究方法:在这项三期研究中,受试者被随机分配接受elotuzumab加来那度胺和地塞米松(elotuzumab组)或来那度胺加地塞米松(对照组)治疗。复合观察终点是无进展生存期和总反应率。其最终结果是根据无进展生存期的中期分析产生的。
研究结果:Elotuzumab组纳入321名患者,对照组纳入325名。24.5个月的中位随访后,Elotuzumab组和对照组的一年无进展生存率分别为68%和57%;两年无进展生存率分别为41%和27%。Elotuzumab组的中位无进展生存期为19.4个月,对照组为14.9个月(elotuzumab组进展或死亡的风险率为0.70;95%CI 0.57-0.85;p<0.001)。Elotuzumab组和对照组的总缓解率分别为79%和66%(P<0.001)。两组常见的3、4级不良反应有淋巴细胞减少症、中性粒细胞减少症、疲乏和肺炎。Elotuzumab组有33个病人(10%)出现输液反应,其中29个人被评为1或2级。
研究结论:复发性/难治性多发性骨髓瘤患者接受Elotuzumab、来那度胺、地塞米松联合治疗可将疾病进展或死亡的风险降低30%。
原始出处:
Sagar Lonial, Meletios Dimopoulos, et al.Elotuzumab Therapy for Relapsed or Refractory Multiple Myeloma.N Engl J Med 2015; 373:621-631August 13, 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#多发性#
33
#elotuzumab#
30
#mAb#
28
#复发性#
29
#复发性/难治性多发性骨髓瘤#
34
#难治性#
30