Eur J Endocrinol:唑来膦酸可以更好的改善原发性甲状旁腺功能亢进术后患者的骨质疏松
2021-08-25 MedSci原创 MedSci原创
唑来膦酸是双磷酸盐类药物,其主要的功效就是抑制破骨细胞的活性,在临床上常用于治疗恶性肿瘤的骨转移,但对于骨质疏松也有非常明显的治疗作用。正确应用唑来膦酸能够明显的延缓骨吸收,恢复成骨和破骨的动态平衡。
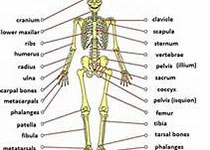
甲状旁腺是位于甲状腺后,即颈部甲状腺后侧,四个像黄豆大小的四个腺体,甲状旁腺虽然腺体最小,但是功能巨大,调节着骨骼的钙磷代谢。这个腺体主要分泌甲状旁腺激素,甲状旁腺激素分泌过多,会把骨骼的钙、矿物质吸收入血,通过尿排出来,引起骨质疏松,这就是甲状旁腺功能亢进性骨质疏松症,表现为钙磷代谢异常,最后导致严重的骨质疏松和骨折,严重者引起纤维囊性骨炎等一系列表现。
唑来膦酸是双磷酸盐类药物,其主要的功效就是抑制破骨细胞的活性,在临床上常用于治疗恶性肿瘤的骨转移,但对于骨质疏松也有非常明显的治疗作用。正确应用唑来膦酸能够明显的延缓骨吸收,恢复成骨和破骨的动态平衡,从而达到抗骨质疏松的作用。
本文就来解读一下原发性甲状旁腺功能亢进术后骨质疏松的患者使用唑来膦酸与否的结局是否有明显差异。
目的:原发性甲状旁腺功能亢进(PHPT)合并骨质疏松症患者行甲状旁腺切除术后骨密度(BMD)可以得到改善。目前尚不清楚手术联合术后双磷酸盐治疗是否能进一步改善骨骼健康。这项随机对照研究比较了单独手术和术后联合唑来膦酸对PHPT合并骨质疏松患者骨代谢的影响。
方法:56例PHPT和骨质疏松患者(f/m 47/9,平均年龄68.4岁)在甲状旁腺切除术后1-3个月随机接受唑来膦酸或安慰剂治疗两年。共计随访2年,每年测量双能X线骨密度(DXA)和骨转换标志物(1型前胶原N端前肽、1型胶原C端肽和碱性磷酸酶)。
结果:甲状旁腺切除术后2年,唑来膦酸(ZOL)组与安慰剂(PBO)组相比,股骨颈(Z值P = 0.045)和腰椎(T值和Z值的P值分别为P = 0.039和P =0.017)的BMD显著升高。
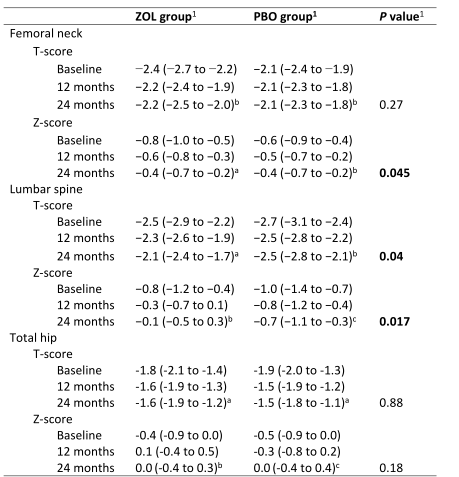
表1 校正术前双膦酸盐治疗后,ZOL组(n = 28)和PBO组(n = 28)在甲状旁腺切除术后骨密度的变化
数据显示为基于模型的平均值(95% CI)
aP < 0.001, bP < 0.01, cP < 0.05 观察各组24个月以上的治疗效果,粗体P值表示P < 0.05
骨转换指标在ZOL组显著降低(P < 0.001)。
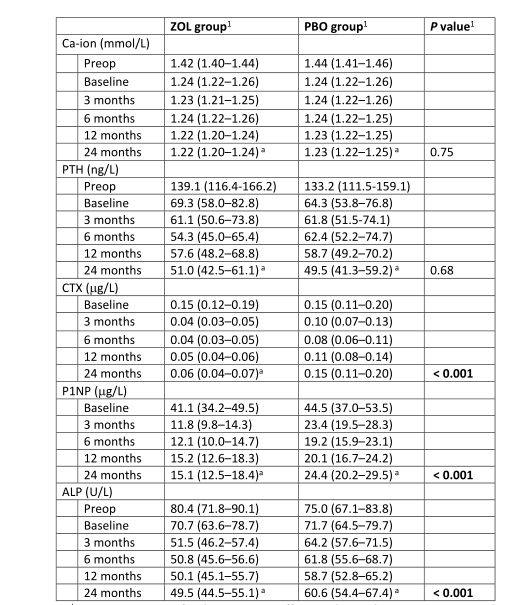
表2 校正术前双膦酸盐治疗后,ZOL (n = 28)组和PBO (n = 28)组甲状旁腺切除术后的生化变化。
数据显示为基于模型的平均值
aP < 0.001, bP < 0.01, cP < 0.05 观察各组24个月以上的治疗效果,粗体P值表示P < 0.05
在术前>1年接受双膦酸盐治疗的18例患者中,ZOL组股骨颈和腰椎的BMD均有显著改善(N = 10;所有P < 0.001-0.01),而PBO组仅在腰椎有改善(N = 8, P= 0.03), (组间差异P= 0.08-0.95)。
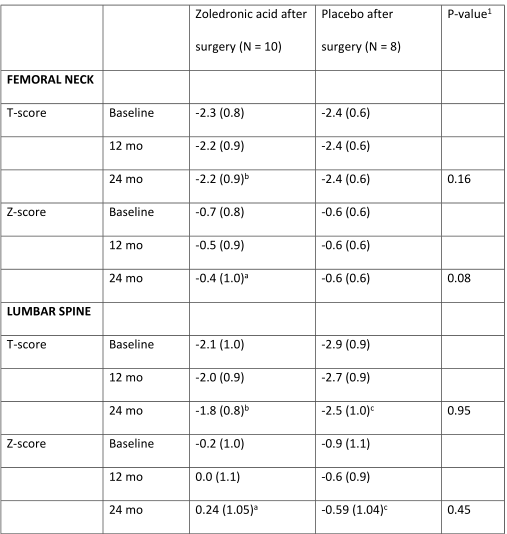
表3 术前双膦酸盐患者甲状旁腺切除术后DXA测量值的变化(N = 18)。
aP < 0.001, bP < 0.01, cP < 0.05 观察各组24个月以上的治疗效果,粗体P值表示P < 0.05。
结论:甲状旁腺切除术后,无论是否使用唑来膦酸,骨密度均增加,但术后使用唑来膦酸后骨密度增加的更为显著。
原始出处
Ryhänen EM, Koski AM, Löyttyniemi E, Valimaki MJ, Kiviniemi U, Schalin-Jantti C. Postoperative Zoledronic Acid for Osteoporosis in Primary Hyperparathyroidism: a Randomized Placebo-controlled Study. Eur J Endocrinol. 2021 .
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#原发性#
53
#甲状旁腺功能亢进#
36
#唑来膦酸#
35
#甲状旁腺#
42
#原发性甲状旁腺功能亢进#
39
#骨质#
27
骨代谢方面的文章好好学习一下
41