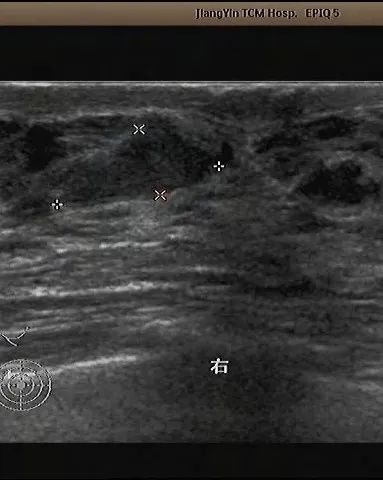
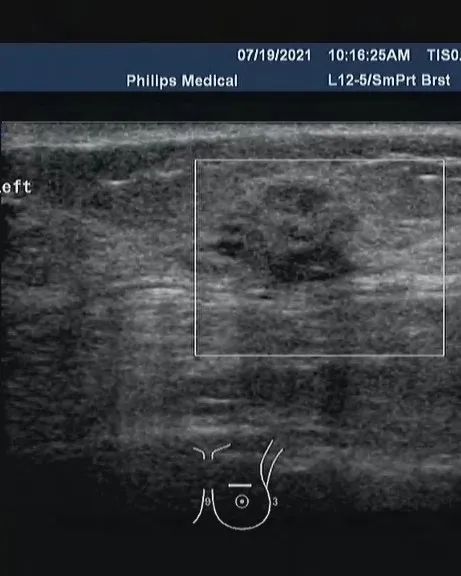
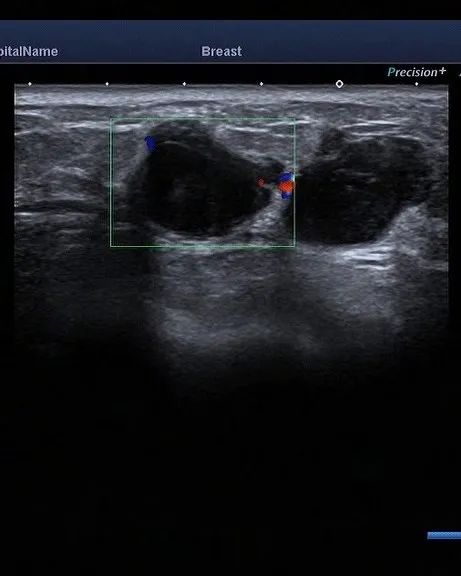
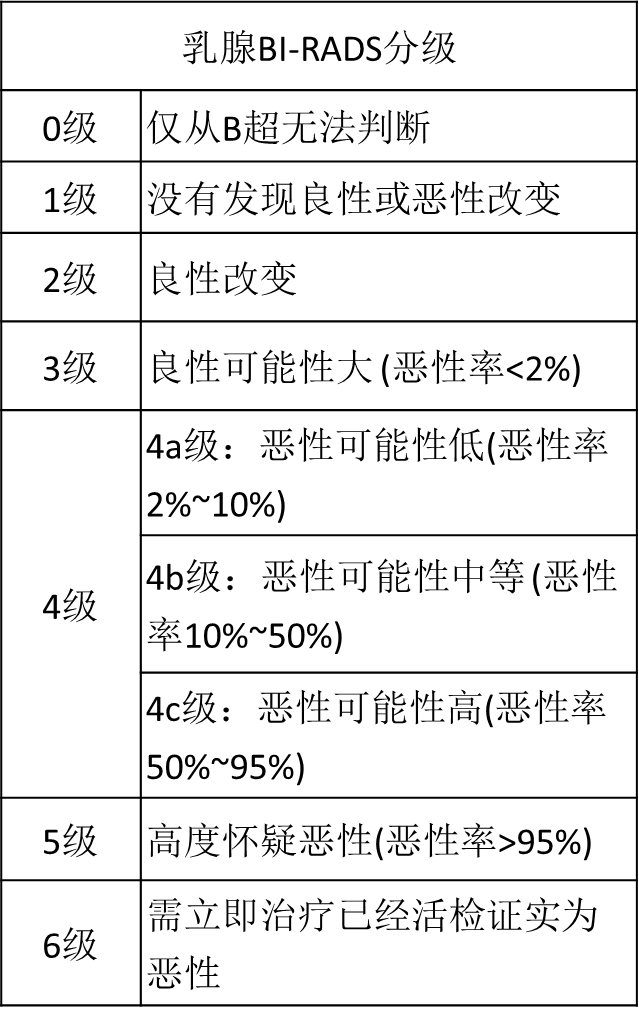
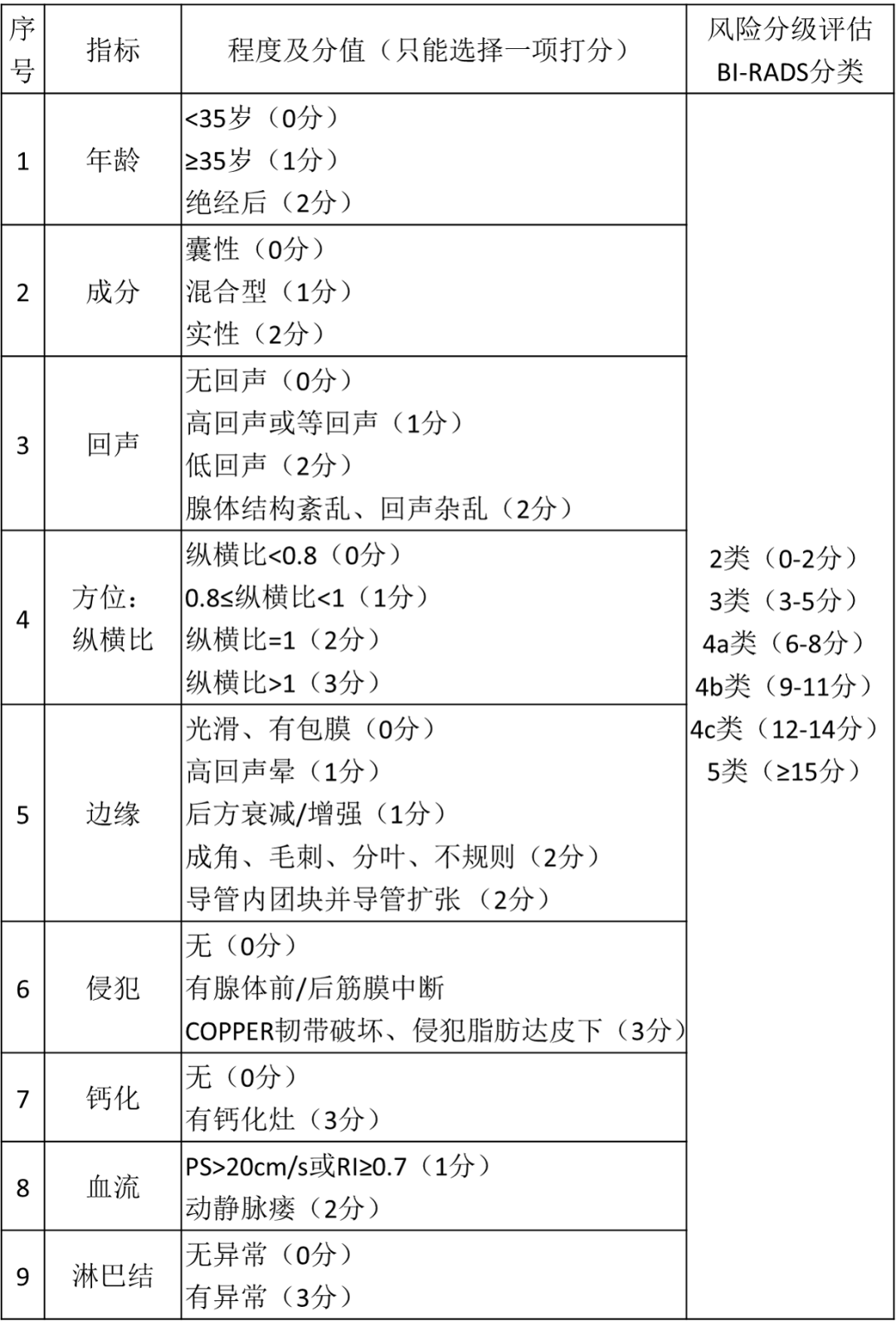
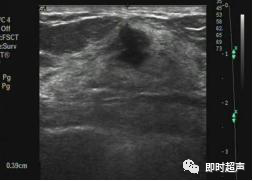
乳腺结节的发病率现在越来越高,大部分实性的乳腺结节主要是超声检查发现的低回声病灶,经常良性比较多。但也有一部分是乳腺癌,所以,乳腺结节分级尤为重要。 乳腺结节的分级是什么? 一旦彩超发现乳腺结节,就会根据乳腺结节的形状,进行一次面试进行评级,也即是对其的危险度进行评分,BI-RADS分级法将乳腺病变分为0~6级,一般来说,级别越高,恶性的可能性越大。 边界比较清楚的、漂亮规整的会归类 2 级或 3 级,考虑为比较好的结节,危险性不高; 边界没那么清楚、不漂亮的、形状没那么规则的可能归为 4A 级,表示这个结节有点轻微的怀疑,需要进一步检查证明它是不是好结节。当然随着形态的不好,危险度的升高,还有 4B 级,4C 级,5 级,6 级的评分。 BI-RADS是美国放射学会的乳腺影像报告和数据系统(Breast Imaging Reporting and Data System)的缩写。BI-RADS 分级标准是由美国国家癌肿研究所、美国疾病控制预防中心、美国食品药品管理局、美国医学会、美国外科医师学会和美国病理学家学会、美国放射学会共同努力制定的。这一标准的建立使描述乳腺病灶的特征性术语和评价病灶恶性程度的报告术语趋于标准化规范化,降低了解读乳腺影像学报告中出现误差和不确定性,尤其对乳腺癌复查诊断更为重要。 该分级主要从形态、方位、边缘、内部回声、后方特征、与周围组织关系、钙化等几方面描述乳腺肿物。 形态不规则、纵横比大于1、边缘模糊(成角、微小分叶、“蟹足状突起”)、不均质低回声、后方回声改变、结构紊乱侵犯周边组织、钙化均考虑为恶性标志。 单纯性囊肿、积乳囊肿;乳房内移植物; 稳定的术后改变; 随访后无变化的纤维腺瘤。 包括边缘光整、呈圆形或椭圆形、横径大于高径的实性肿块,很可能是纤维腺瘤; 触诊阴性的复杂囊肿和簇状微囊肿。




本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ADS#
67
#RADS#
54
#BI-RADS#
45
#乳腺结节#
66
分类catogary 分级grade 这俩词还是有些微区别的吧
62
学习可
53