Hypertension:钠饮食摄入与肾钠处理功能的相互作用可影响血压
2013-09-03 佚名 丁香园
图1.不同的锂排泄分数三分位组中,夜间舒张压与钠排泄的关系。 图2.夜间收缩压与钠饮食摄入与肾钠处理功能的相互作用的关系。 研究要点: 钠饮食摄入和近端肾小管的钠处理功能相互作用,从而影响血压水平。 低钠饮食对于控制血压及降低肾功损害都有着长远的益处。 大量的研究指出钠摄入量与血压水平相关,但是,这种相关度在个体之间存在明显的差异,且多种因素可影响两者的相关性强度。为此,
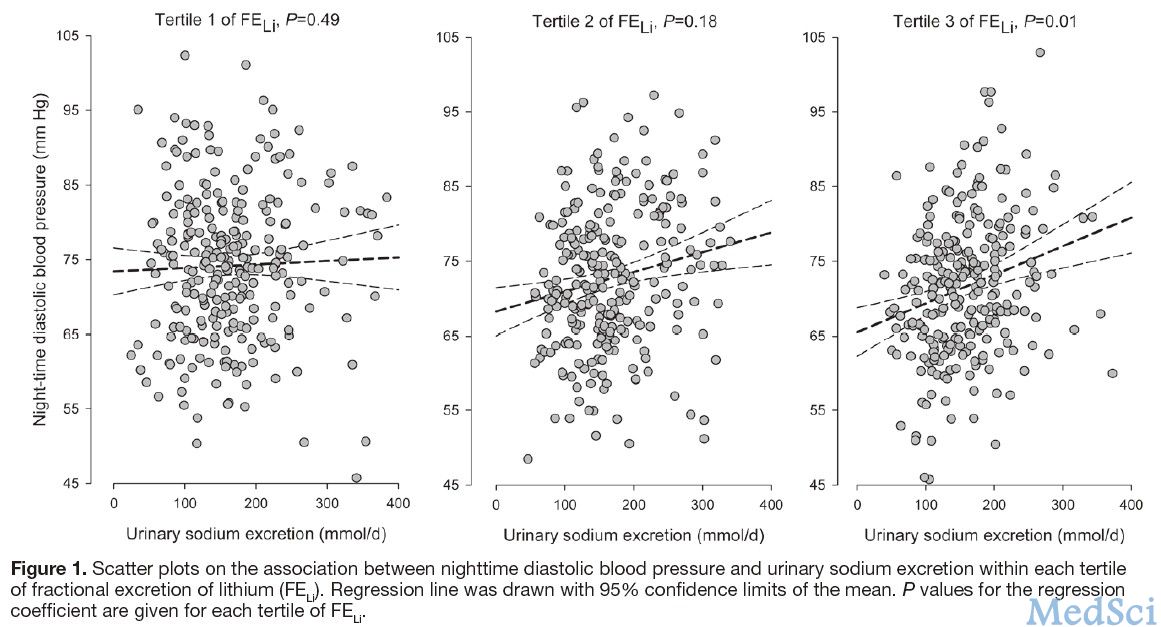
图1.不同的锂排泄分数三分位组中,夜间舒张压与钠排泄的关系。
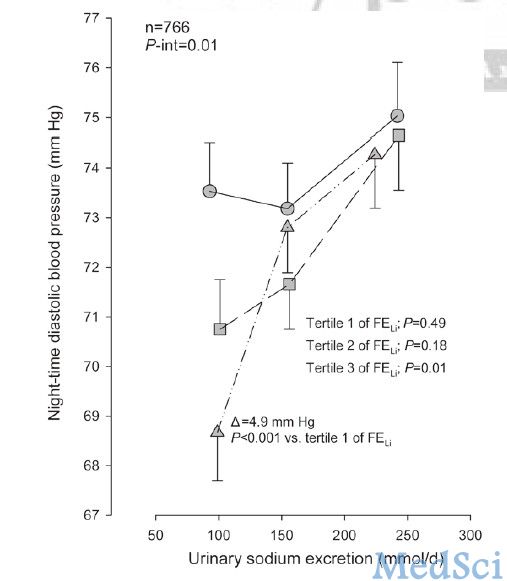
图2.夜间收缩压与钠饮食摄入与肾钠处理功能的相互作用的关系。
研究要点:
钠饮食摄入和近端肾小管的钠处理功能相互作用,从而影响血压水平。
低钠饮食对于控制血压及降低肾功损害都有着长远的益处。
大量的研究指出钠摄入量与血压水平相关,但是,这种相关度在个体之间存在明显的差异,且多种因素可影响两者的相关性强度。为此,来自上海交通大学瑞金医院王继光等从钠饮食摄入与肾钠处理功能的关系为研究点进行了相关临床试验,研究发现钠饮食摄入与肾钠处理功能的相互作用可影响血压。该研究论文发表于8月Hypertension杂志。【原文下载】
研究人员选取了766名受检者,其中男性379名,动态血压异常患者478名;有697名受检者从未接受过降压药物治疗,69名超过两周未接受降压药物治疗。研究测量了24小时尿钠排泄及内源锂清除率来分别评估钠饮食摄入与肾钠处理功能,同时,研究者测量了锂排泄分数及远端的钠重吸收率分别作为近端和远端的肾钠处理功能参数。
调整处理后统计结果显示尿钠排泄,锂排泄分数及远端钠重吸收分数等因素与临床或动态血压水平并没有明显的相关性;但是,在夜间舒张血压方面,尿钠排泄和锂排泄分数有明显的相互影响作用。除去锂排泄分数三分位组的1号组,在其余两组,夜间舒张血压与尿钠排泄成正相关;然而,锂排泄分数1号组的夜间舒张血压水平要明显高于3号组,而且在钠排泄分数的最低组更为明显。在夜间收缩血压,临床或动态24小时血压方面也有相似的趋势。
王继光等人认为该研究指出了钠饮食摄入和近端肾小管的钠处理功能相互作用,从而影响血压水平。低钠饮食对于控制血压及降低肾功损害都有着长远的益处。
原文下载
Zou J, Li Y, Yan CH, Wei FF, Zhang L, Wang JG.Blood Pressure in Relation to Interactions Between Sodium Dietary Intake and Renal Handling.Hypertension. 2013 Aug 19.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TENS#
33
#相互作用#
42
#PE#
35
#互作#
51
#Hypertension#
24