Lancet:常规插管后的张力性水气心包
2015-05-04 MedSci MedSci原创
2014年6月,一个患有晚期肾病和慢性尿毒症心包积液的37岁病人来到我们机构,伴随逐渐恶化的呼吸困难和端坐呼吸,肾切除手术4天后控制高血压。他在拒绝移植肾的前9年每周3次定期进行血液透析。检查静息时病人出现严重呼吸困难,脉搏102次每分钟,呼吸率20次每分钟,血压110/70 mm Hg,伴有25mm Hg诡异变化。肺听诊显示基部支气管呼吸声。胸部X线表明有气-液水平的心脏肥大。胸部CT显示心包积
2014年6月,一个患有晚期肾病和慢性尿毒症心包积液的37岁病人来到我们机构,伴随逐渐恶化的呼吸困难和端坐呼吸,肾切除手术4天后控制高血压。他在拒绝移植肾的前9年每周3次定期进行血液透析。检查静息时病人出现严重呼吸困难,脉搏102次每分钟,呼吸率20次每分钟,血压110/70 mm Hg,伴有25mm Hg诡异变化。肺听诊显示基部支气管呼吸声。胸部X线表明有气-液水平的心脏肥大。胸部CT显示心包积水充气。超声波心动描记术显示巨大心包渗漏引起二尖瓣流入超过25%的呼吸变异,与心包填塞生理学一致。我们做了一个心包窗口,并流出大概1L的血清血液流体。心包液培养为阴性,心包活组织检查分析显示急性和慢性炎症和纤维化。治疗性引流后病人住院治疗情况平静。2周后,后续超声波心动描记术显示只有轻微心包积液。在2014年12月,病人好了,超声波心动描记术显示只有轻微心包积液。2015年3月,病人状态良好,但在纳马齐教学医学继续保持血液透析。

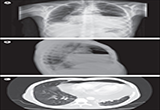
Figure Hydropneumopericardium
Posteroanterior (A) and lateral (B) chest radiographs showing cardiomegaly with an air–fluid level at the heart level. (C) Transverse CT showing hydropneumopericardium.
心包积气通常发生在钝挫伤或穿透性胸外伤后,但是偶尔也会发生于插管和机械通风。除了最近肾切除术插管外,我们没有发现病人其它风险因素。心包积气极少叠加于已存在心包积液而导致紧张性水气心包,像我们的病人这样。普通放射成像类似于大量食管裂孔疝或胃扭转;包含气液水平的心脏边界描绘有助于排除这些鉴别诊断。
原始出处:
Prof Mohammad Ali Ghayumi, MD, Dr Mohammad Javad Fallahi, MD, Seyed Masoom Masoompour, MD, Prof Jamshid Roozbeh, MD.Tension hydropneumopericardium after routine intubation. Lancet, April 30, 2015. DOI: http://dx.doi.org/10.1016/S0140-6736(15)60028-9
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








特殊病例学习了。
103
#Lancet#
25
#张力#
29