Nature Communications:以毒攻毒!得过感冒,对减少新冠感染真的有帮助!
2022-01-30 生物碳素 生物碳素
在引起我们感冒的病毒中,其中有一部分属于冠状病毒,这些冠状病毒能够引起免疫系统的防御和攻击,使体内免疫T细胞能够轻易识别出新冠病毒,进而实现对人体的免疫保护。
在引起我们感冒的病毒中,其中有一部分属于冠状病毒,这些冠状病毒能够引起免疫系统的防御和攻击,使体内免疫T细胞能够轻易识别出新冠病毒,进而实现对人体的免疫保护。并且,以往也有研究表明其他冠状病毒诱导的T细胞能够识别SARS-CoV-2。
最近,在伦敦帝国理工学院的一项研究中,研究人员首次试验了当人类暴露于SARS-CoV-2时,这些被其他冠状病毒诱导的T细胞是如何影响人类感染新冠可能性的。
相关研究结果以“Cross-reactive memory T cells associate with protection against SARS-CoV-2 infection in COVID-19 contacts”为题,发表在Nature Communications上。
图1. 研究成果(图源:Nature Communications)
研究人员之一Rhia Kundu博士说,有些人即使暴露于SARS-CoV-2也不会感染病毒,至于究竟是什么原因,至今尚未可知。这或许是因为人体在此之前感染过其他类型的冠状病毒,它们所诱导产生的交叉反应性T细胞能够保护这部分人,使得他们不会轻易感染新冠病毒。
在这项研究中,一共有52名因与SARS-CoV-2感染者共同生活而接触该病毒的参与者被纳入试验,参与者们分别在开始试验之前、试验4天后及试验7天后接受了PCR检测,以确认是否出现病毒感染。在试验期间经过病毒检测,结果显示26人感染新冠病毒,26人尚未感染。
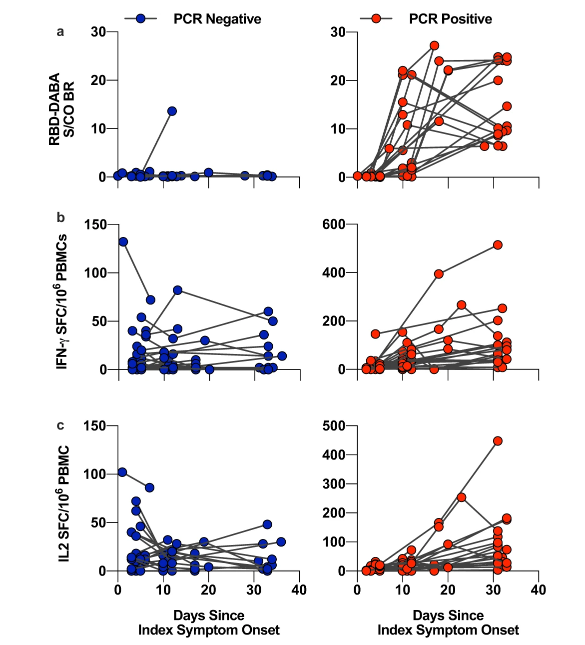
图2. PCR阳性和阴性接触者体内交叉反应性T细胞及RBD特异性抗体的动态变化(图源:Nature Communications)
在参与者暴露于新冠病毒后的1-6天内,研究人员采集了他们的血液样本,分析了参与者因感染其他冠状病毒而诱导的预存T细胞水平,这类T细胞被证明可以识别新冠病毒的内部蛋白。研究人员发现,与感染新冠的26人相比,尚未感染的26人体内交叉反应性T细胞的水平明显更高,感染了新冠的接触者体内完全不存在此类T细胞,这类保护性T细胞主要靶向新冠病毒内部的非刺突蛋白,进而防止病毒感染。
目前,市场上的新冠疫苗主要针对病毒表面的刺突蛋白,不会诱导对病毒内部蛋白质的免疫反应,而经过其他冠状病毒诱导的这些T细胞,其目标是新冠病毒的内部蛋白。
因此,研究人员指出,除了我们现有的刺突蛋白靶向疫苗之外,这些内部蛋白提供了一种新的疫苗靶点,可以为人体提供更持久的免疫防护作用。因为T细胞反应持续时间比抗体反应持续时间更长,抗体反应在接种疫苗后几个月内就会减弱。
“刺突蛋白承受着来自疫苗诱导抗体的强烈免疫压力,推动了疫苗逃逸突变体的进化。相比之下,我们发现保护性T细胞靶向的内部蛋白质,其突变的可能性要少的多。所以,靶向病毒内部蛋白质的疫苗能够有效应对当前和未来的SARS-CoV-2变体”,伦敦帝国理工学院的医学博士AjitLalvani说。
综上,这项研究表明,其他冠状病毒诱导产生的交叉反应T细胞可以保护人体免受新冠病毒感染。值得一提的是,由于交叉反应T细胞的目标是病毒内部蛋白质而不是刺突蛋白,所以这项研究也提供了一个新的新冠疫苗靶点,在二代疫苗中若能够加入非刺突抗原,或可大大增强疫苗效果。
参考资料:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#COMMUN#
29
#以毒攻毒#
40
#Nat#
27
#Nature Communications#
33