JCO:术中冰冻病理诊断指导亚肺叶切除术精准切除
2015-12-04 MedSci MedSci原创
复旦大学附属肿瘤医院胸部肿瘤多学科综合诊治团队准确描述并定义了周围型肺腺癌的术中冰冻病理诊断,同时以此提出了兼具微创、精准和疗效三位一体亚肺叶切除手术方式的精准指征。相关成果日前在线发表于《临床肿瘤学杂志》。据上述团队首席专家陈海泉介绍,团队中的放射介入医师在CT的精确引导下,为每一例肺小结节患者通过胸外插入“带钩钢丝”,从而为外科医生术中精确找到病灶作好“位置标记”。此项技术开展近8年来,已完成
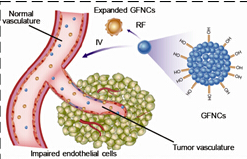
复旦大学附属肿瘤医院胸部肿瘤多学科综合诊治团队准确描述并定义了周围型肺腺癌的术中冰冻病理诊断,同时以此提出了兼具微创、精准和疗效三位一体亚肺叶切除手术方式的精准指征。相关成果日前在线发表于《临床肿瘤学杂志》。
据上述团队首席专家陈海泉介绍,团队中的放射介入医师在CT的精确引导下,为每一例肺小结节患者通过胸外插入“带钩钢丝”,从而为外科医生术中精确找到病灶作好“位置标记”。此项技术开展近8年来,已完成患者1000余例,定位精准率达99%以上;同时,由于取下的病变组织完整,为病理科作出明确诊断创造了条件。
“术中,我们不仅追求手术切口的大小、打洞的数量,更关键的是能根据术中的病理结果精准地进行病变组织切除,减少术中器械游离时对正常组织造成的伤害。”陈海泉表示。
据统计,肿瘤医院在国内率先开展全腔镜下Ivor Lewis食管癌根治术、胸腔镜下肺癌根治术、保留肌肉的小切口开胸肺叶切除术等微创手术。目前,累计完成超过1万多例胸部肿瘤微创手术。
陈海泉介绍说,此项成果具有里程碑意义:“首先,精确的术中冰冻病理诊断对于早期周围型肺腺癌患者手术方式的选择具有重要指导价值;其次,对于复发低危的周围型肺腺癌患者,行亚肺叶切除术可在保证疗效的前提下,精确划定手术范围,将内部脏器的损伤降至最低,从而最大程度地保留肺功能,提高手术安全性。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#亚肺叶#
43
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
70
#JCO#
46
#切除术#
28
好文章,值得收藏
158
历害
94
#病理诊断#
37
#精准#
22
#肺叶切除#
38
号
72