肠道微生物又上头条了!看克利夫兰诊所在《cell》上的发文
2015-12-30 周伦 奇点网
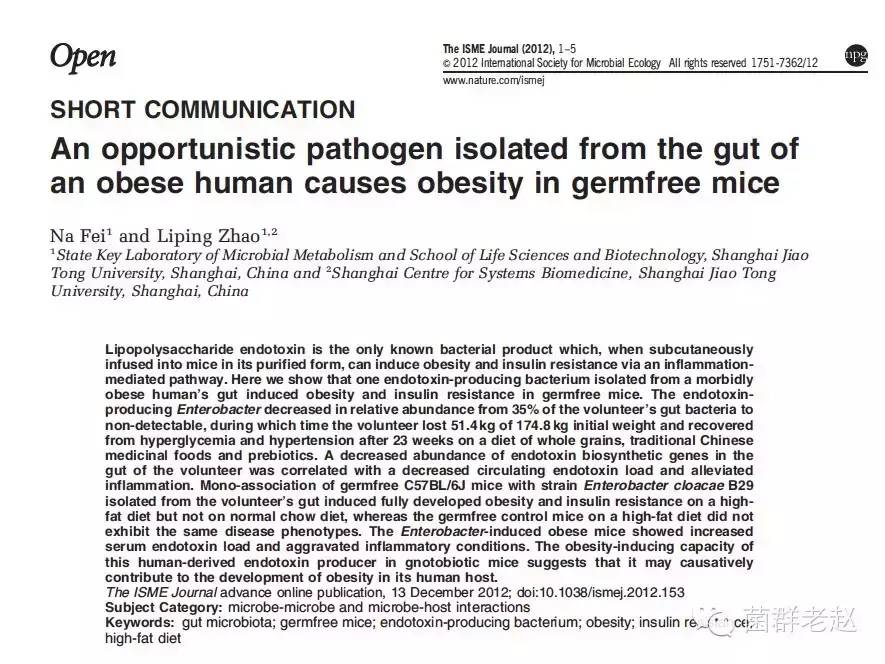
现实生活中,人们总是难以抵制脂肪的诱惑,因为它是如此的爽滑鲜香。有人辩解说,人类嗜脂肪是基因对远古饥饿的记忆造成的。现在饥饿终于不再缠着我们了,可是心血管疾病却找上了门。据WHO统计,每年大约有1750万人死于心血管疾病,竟占到全年死亡总人数的三分之一。众所周知,动脉粥样硬化是心血管疾病发作的主要因素之一。而高脂饮食恰恰是动脉粥样硬化的罪魁祸首。最近有研究表明,动脉粥样硬化背后的“主谋”之一竟是肠
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
24
#CEL#
21
#微生物#
30
呵呵,好诙谐
127
谢谢分享,
160
不错,
97
哦
112
嗯,
79
好文章,
92
赞一个!!
89