JBJS:踝关节骨折内固定治疗术后伤口并发症的风险因素
2012-12-06 JBJS JBJS
据人口统计学调查研究显示,踝关节骨折内固定术后的总体并发症发生率为5%-40%,伤口并发症发生率为1.4%-18.8%。以往的大部分研究多集中在再次住院患者的并发症情况,很少有研究考察大多数门诊病例的伤口并发症风险因素。 最近,美国宾夕法尼亚州托马斯·杰弗逊大学医院Rothman医学研究所的Adam G. Miller, MD等实施了一项临床观察研究,通过对住院及门诊患者的追踪考察,对患者踝关节
据人口统计学调查研究显示,踝关节骨折内固定术后的总体并发症发生率为5%-40%,伤口并发症发生率为1.4%-18.8%。以往的大部分研究多集中在再次住院患者的并发症情况,很少有研究考察大多数门诊病例的伤口并发症风险因素。
最近,美国宾夕法尼亚州托马斯·杰弗逊大学医院Rothman医学研究所的Adam G. Miller, MD等实施了一项临床观察研究,通过对住院及门诊患者的追踪考察,对患者踝关节骨折内固定术后的伤口并发症发生风险进行分析,他们的研究结果发表在最新一期的J Bone Joint Surg Am上,其证据级别为预后性研究I级。
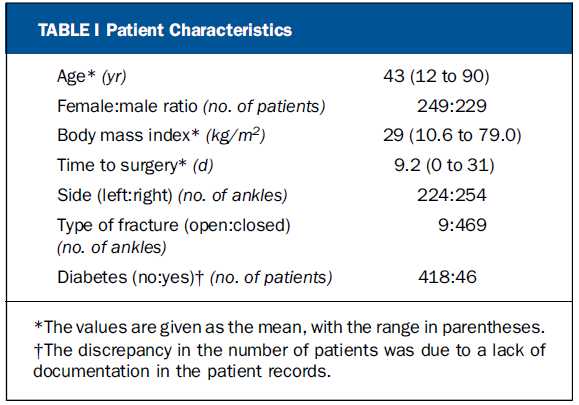
2003年至2010年间因踝关节骨折接受切开复位内固定治疗的478例患者纳入本研究,所有患者的内固定手术在同一医疗机构,并由同一手术医生实施。随访中,对患者的人口统计学数据,手术时间,伴发疾病以及术后护理等变量进行评估分析。对于需要进行换药处理、口服抗生素或进一步手术治疗的患者,定义为伤口并发症发生病例。
研究结果显示,478例患者均获得随访,其中6例(1.25%)出现伤口并发症的患者需实施手术清除处理,14例(2.9%)需进行伤口换药处理或口服应用抗生素治疗。糖尿病史(p < 0.001),周围神经病变(p = 0.003),伤口局部用药(p = 0.011),开放性骨折(p = 0.05)以及术后治疗不配合(p = 0.027)等因素与伤口并发症呈显著相关关系。出现伤口并发症的患者与无伤口并发症的患者在年龄分布上存在较大的显著差异(p = 0.045)。手术时间与伤口并发症之间未见显著相关关系。
表1.患者的一般资料
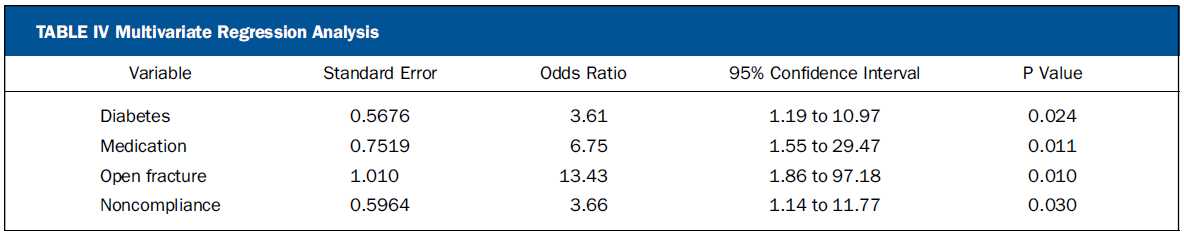
该研究结果表明,踝关节骨折病例采取切开复位内固定治疗术后,为了防止出现伤口并发症问题,积极处理患者复杂的内科疾病非常重要;另外,对于术后不配合治疗的病例应特别提起注意。随着损伤部位肿胀处理的加强,手术时间不会显著影响患者的伤口愈合情况,临床医生应重视对治疗失败患者的术后监管。
表2.伤口并发症的风险因素
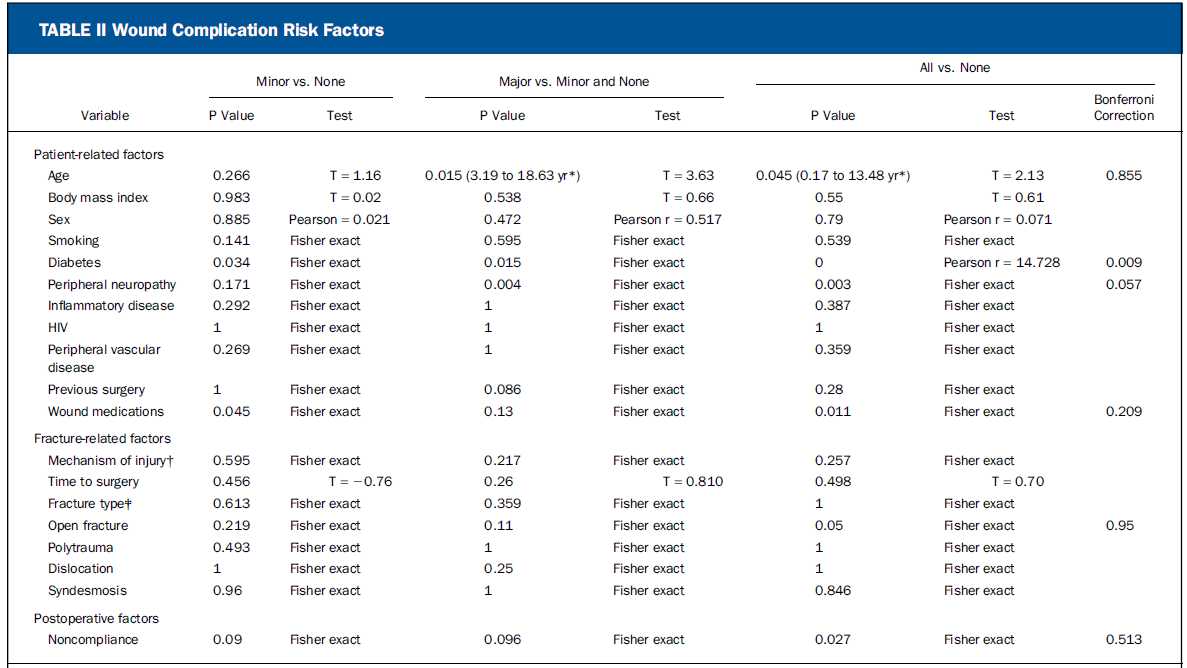
表3.回归分析:任何伤口并发症问题的优势比计算结果
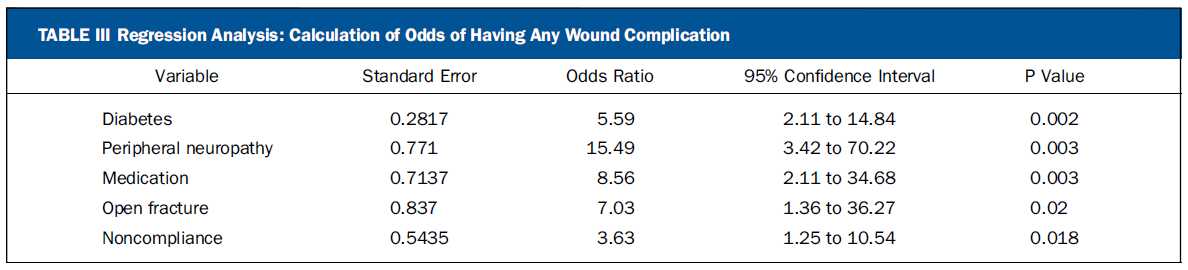
表4.多变量回归分析结果

Background:
The overall rate of complications after ankle fracture fixation varies between 5% and 40% depending on the population investigated, and wound complications have been reported to occur in 1.4% to 18.8% of patients. Large studies have focused on complications in terms of readmission, but few studies have examined risk factors for wound-related issues in the outpatient setting in a large number of patients. A review was performed to identify risk factors for wound complications tracked in the hospital and outpatient setting.
Methods:
Four hundred and seventy-eight patients underwent open reduction and internal fixation of an ankle fracture between 2003 and 2010 by a single surgeon at a single institution. Demographic characteristics, time to surgery, comorbidities, and postoperative care were tracked. Wound complications were defined as those requiring dressing care and oral antibiotics or requiring further surgical treatment.
Results:
Of the 478 patients who were followed, six (1.25%) had wounds requiring surgical debridement. Fourteen patients (2.9%) required further dressing care or a course of oral antibiotics. There were significant associations between wound complications and a history of diabetes (p < 0.001), peripheral neuropathy (p = 0.003), wound-compromising medications (p = 0.011), open fractures (p = 0.05), and postoperative noncompliance (p = 0.027). There was a significant difference in age between patients with and without wound complications (p = 0.045). We did not identify a relationship between time to surgery and complications.
Conclusions:
These results highlight the difficulty of treating medically complex and noncompliant patient populations. With careful preoperative monitoring of swelling, time to surgery does not affect wound outcome. The failure of the patient to adhere to postoperative instructions should be a concern to the treating surgeon.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#骨折内#
123
#并发#
37
好文章
123
#踝关节骨折#
54
#踝关节#
36
#内固定#
25
#JBJS#
26