自发孤立性肠系膜上动脉夹层丨CT平扫征象
2022-08-02 熊猫放射 网络
总之,对急诊腹痛患者的腹部CT平扫中,存在SMA主干扩张的征象,特别是当扩张的SMA主干直径超过10mm时,应高度怀疑SISMAD。
-
为了测量准确,每例SMA 主干CT值和直径测量位置在SMA主干最宽处,测量三次取平均值。 -
SMA主干扩张的定义为SMA 主干直径>9mm。 -
SMA管壁的弧形高密度征定义为SMA管壁出现高于同层面腹主动脉管壁弧形密度。 -
管壁钙化定义为SMA管壁出现>140HU的致密影。 -
管壁周围脂肪浑浊定义为SMA管壁周围脂肪密度增加、模糊。
CT征象
中国人正常肠系膜上动脉主干直径一般<9mm。本研究发现SMA主干扩张是SISMAD最具有诊断意义的征象 。SISMAD真、假腔形成,假腔管壁由于缺乏弹性层,容易扩大,导致SMA直径长范围明显扩张。
SMA周边脂肪浑浊为一种渗出性改变,SMA管壁的高密度可能与管壁的出血有关,这2种征象可随病程发生变化。SMA管壁周脂肪浑浊征象出现的机率除疾病因素( 如炎症、肿瘤及其他血管性疾病等) 外,可能还与病程的检查时间点有关,特别是在急性期,更容易被发现,到病程后期出现概率明显减低。
SMA管壁密度增高征象可能还与SMA夹层的类型有关,管壁密度高低征象还容易受到评判人的主观因素影响。SISMAD管腔CT值密度一般偏高,这可能与夹层中假腔血流缓慢或新鲜血栓形成有关。但单从SMA管壁和管腔的密度改变难以诊断SISMAD。
鉴别诊断
SMA动脉瘤常呈梭形和局限性扩张,直径常超过15mm,动脉周边脂肪间隙常清晰,除非动脉瘤破裂可发生脂肪浑浊征象; 而SISMAD常节段性扩张、累及的范围较长,管壁常呈高密度,周边脂肪模糊。
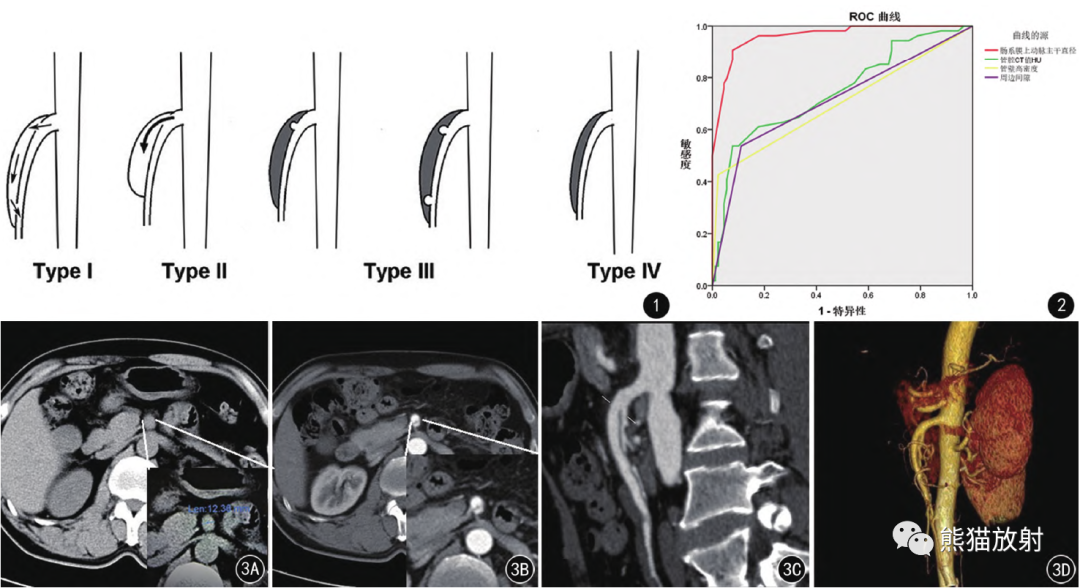
图1 SISMAD的Sakamoto分型: Ⅰ型夹层存在入口与出口; Ⅱ型夹层只有入口,无出口; Ⅲ型假腔已闭塞,近段或/和远段存在穿透性溃疡; Ⅳ型,假腔闭塞。
↓ 内容来源:

感谢作者和期刊!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CT平扫#
44
#动脉夹层#
42
#孤立性#
43
#肠系膜#
45