中国誓言控制滥用抗生素药物
2016-09-06 佚名 参考消息网
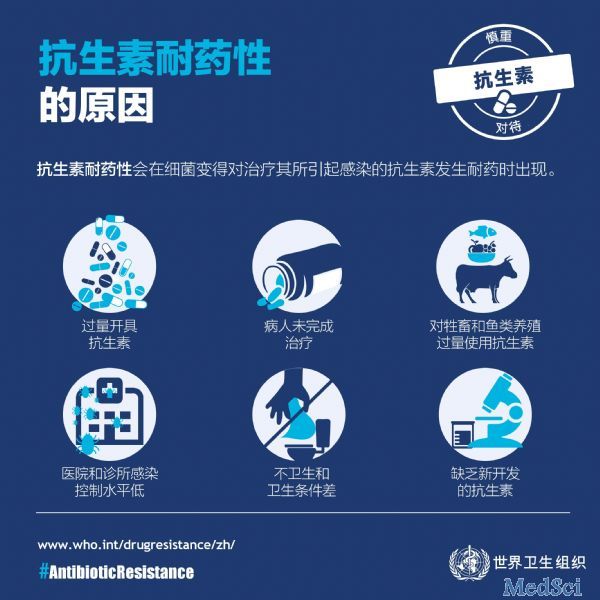
外媒称,中国作为世界人用和兽用抗生素的最大消费国,誓言要加强新型抗菌药物的研发并控制现有药物的过度使用,以应对不断加剧的细菌耐药性问题。据美国《科学》周刊网站8月31日报道,中国中央政府8月26日发布一项国家行动计划,称将调动包括卫生、食品药品和农业等14个部委的力量。政府的目标是,到2020年研发几种新型抗菌药物,凭处方才能销售抗菌药物,加强对人用和兽用抗菌药物使用的监管,加强对医务人员和消费者
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#滥用#
22
继续学习
61
继续关注
59
继续关注
51
继续学习
51